Overview
Polycystic kidney
Polycystic kidney
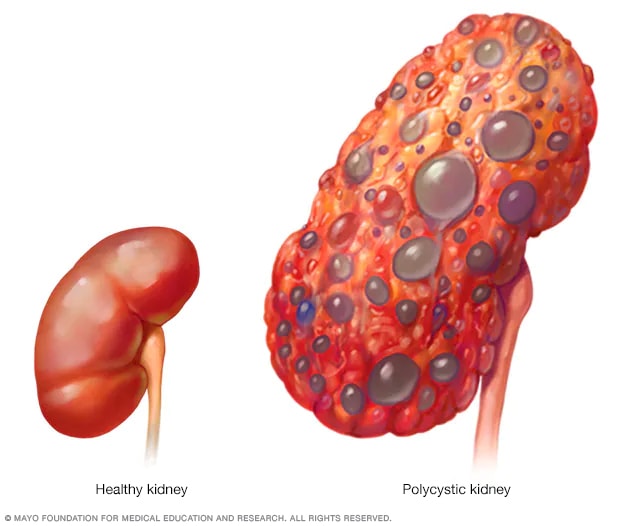
A healthy kidney (left) removes waste from the blood and maintains the body's chemical balance. With polycystic kidney disease (right), fluid-filled sacs called cysts develop in the kidneys. The kidneys grow larger and slowly lose their ability to work as they should.
Polycystic kidney disease (PKD) is a condition in which clusters of cysts grow in the body, mainly in the kidneys. Over time, the cysts may cause the kidneys to get bigger and stop working. PKD is most often passed through families. This is called an inherited condition.
Cysts are round sacs with fluid in them. They are not cancer. In PKD, the cysts vary in size. They can grow very large. Having many cysts or large cysts can damage the kidneys.
Polycystic kidney disease also can cause cysts to grow in the liver, the pancreas and other places in the body. The disease can cause serious complications, including high blood pressure and kidney failure.
PKD varies greatly in how bad it is. It's possible to prevent some complications. Lifestyle changes and treatments might help reduce damage to the kidneys.
Products & Services
Symptoms
Polycystic kidney disease symptoms can include:
- High blood pressure.
- Belly, side or back pain.
- Blood in the urine.
- A feeling of fullness in the belly.
- Increased size of the belly from enlarged kidneys.
- Headaches.
- Kidney stones.
- Kidney failure.
- Urinary tract or kidney infections.
When to see a doctor
People often have polycystic kidney disease for years without knowing it.
If you have some of the symptoms of polycystic kidney disease, see your healthcare professional. If you have a parent, sibling or child with polycystic kidney disease, see your healthcare professional to talk about screening for the condition.
Causes
Autosomal dominant inheritance pattern
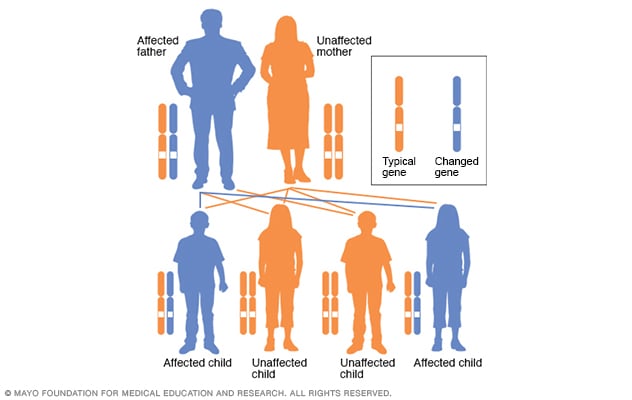
Autosomal dominant inheritance pattern
In an autosomal dominant inheritance pattern, the changed gene is a dominant gene. It's located on one of the nonsex chromosomes, called autosomes. Only one changed gene is needed for someone to be affected by this type of condition. A person with an autosomal dominant condition — in this example, the father — has a 50% chance of having an affected child with one changed gene and a 50% chance of having an unaffected child.
Autosomal recessive inheritance pattern
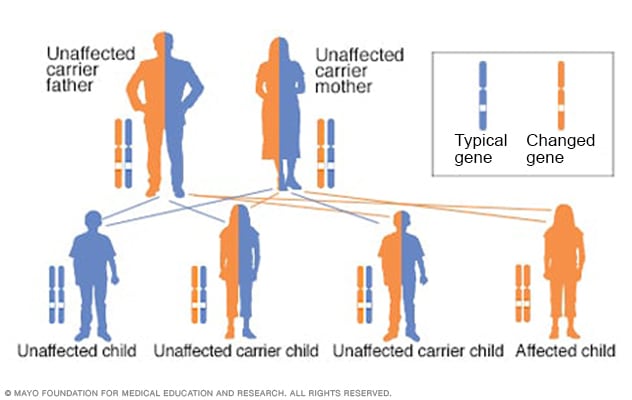
Autosomal recessive inheritance pattern
To have an autosomal recessive disorder, two changed genes, called mutations, are inherited — one from each parent. Their health is rarely affected because they have only one changed gene. Two carriers have a 25% chance of having an unaffected child with two unaffected genes. They have a 50% chance of having an unaffected child who also is a carrier. They have a 25% chance of having an affected child with two changed genes.
Gene changes cause polycystic kidney disease. Most often, the condition runs in families. Sometimes, a gene change happens on its own in a child. This is known as a spontaneous gene change. Then neither parent has a copy of the changed gene.
There are two main types of polycystic kidney disease. They're caused by different gene changes. The two types of PKD are:
-
Autosomal dominant polycystic kidney disease (ADPKD). This is the most common type of ongoing kidney disease that's passed through families, also called inherited. Symptoms of ADPKD often start between the ages of 30 and 40.
Only one parent needs to have the condition to pass it to the children. If one parent has ADPKD, each child has a 50% chance of getting the condition. This is the more common type of polycystic kidney disease.
-
Autosomal recessive polycystic kidney disease (ARPKD). This type is far less common than is ADPKD. The symptoms often appear soon after birth. Sometimes, symptoms don't appear until later in childhood or during the teen years.
Both parents must have gene changes to pass on this form of the condition. If both parents carry a changed gene, each child has a 25% chance of getting the condition.
Risk factors
The biggest risk factor for getting polycystic kidney disease is getting the gene changes that cause the disease from one or both parents.
Complications
Complications linked to polycystic kidney disease include:
- High blood pressure. This is common in polycystic kidney disease. Not treated, high blood pressure can cause more damage to the kidneys and increase the risk of heart disease and strokes.
- Loss of kidney function. The kidneys' losing their ability to do their work is one of the most serious complications of polycystic kidney disease. Nearly half of people with the condition have kidney failure by age 60. But for some people, it starts in the early 30s.
- Pain. It's common to have pain with polycystic kidney disease. Pain often is in the side or back. The pain can come and go or be ongoing. The pain may be linked to bleeding into a cyst, a urinary tract infection, a kidney stone or, less often, cancer.
-
Cysts in the liver. The older people with polycystic kidney disease get, the more likely it is they'll get cysts in the liver. With cysts, the liver most often keeps working.
Women tend to get larger cysts than do men. Hormones and pregnancies might be part of the reason.
-
Brain aneurysm. A balloonlike bulge in a blood vessel, called an aneurysm, in the brain can cause bleeding if it bursts. People with polycystic kidney disease have a higher risk of aneurysms. People with a family history of aneurysms seem to be at highest risk.
Ask your healthcare professional if you need screening. If screening doesn't show an aneurysm, your healthcare professional may suggest screening again in a few years. The timing of repeat screening depends on your risk.
- Pregnancy complications. Most people with polycystic kidney disease can have success with pregnancy. But sometimes, they can get a life-threatening condition called preeclampsia during pregnancy. Those most at risk have high blood pressure or a loss of kidney function before they become pregnant.
- Heart valve conditions. As many as 1 in 4 adults with polycystic kidney disease gets mitral valve prolapse. When this happens, the heart valve no longer closes well. This lets blood leak backward.
- Colon conditions. People with polycystic kidney disease may get weaknesses and pouches or sacs called diverticula in the wall of the colon. This condition is called diverticulosis. Diverticula most often don't cause symptoms, but they may bleed or get infected.
Prevention
If you have polycystic kidney disease and you're thinking about having children, a genetic counselor can help you know your risk of passing the disease to your children.
Keeping your kidneys as healthy as possible may help prevent some of the complications of this disease. It's most important to manage your blood pressure.
Here are some tips for keeping your blood pressure in check:
- Take the blood pressure medicines your healthcare professional prescribes as directed.
- Eat a low-salt diet that has plenty of fruits, vegetables and whole grains.
- Get to and stay at a healthy weight.
- Exercise regularly. Aim for at least 30 minutes of moderate physical activity most days of the week.
- Limit alcohol use.
- Don't smoke.
Aug. 27, 2024