Overview
Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease
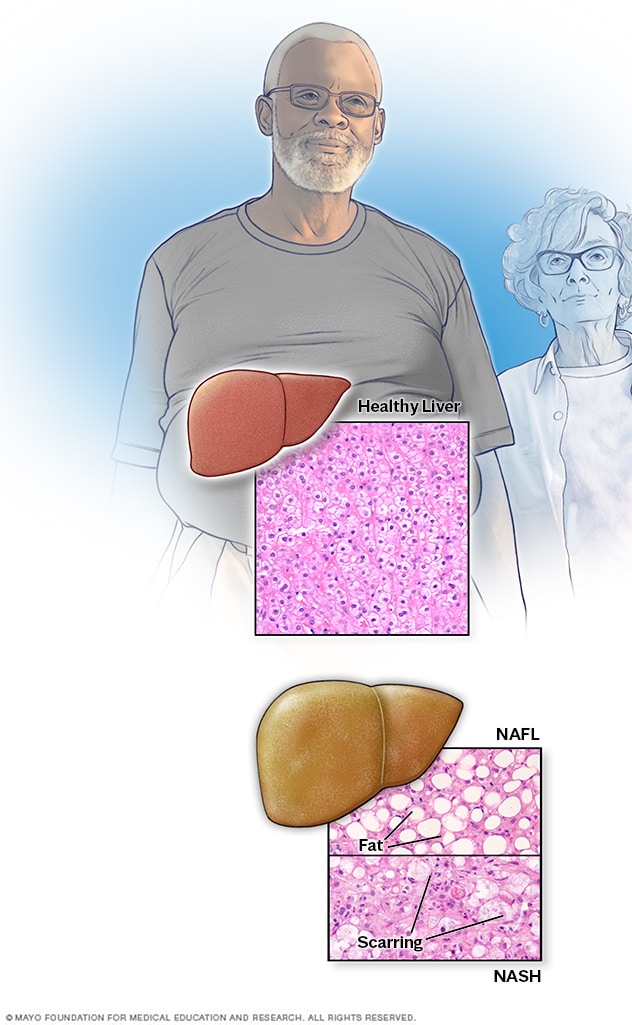
Compared with a healthy liver (top), a fatty liver (bottom) appears bigger and discolored. Tissue samples show extra fat in nonalcoholic fatty liver disease, while inflammation and advanced scarring are seen in nonalcoholic steatohepatitis.
Nonalcoholic fatty liver disease, often called NAFLD, is a liver problem that affects people who drink little to no alcohol. In NAFLD, too much fat builds up in the liver. It is seen most often in people who are overweight or obese.
NAFLD is becoming more common, especially in Middle Eastern and Western nations as the number of people with obesity rises. It is the most common form of liver disease in the world. NAFLD ranges in severity from hepatic steatosis, called fatty liver, to a more severe form of disease called nonalcoholic steatohepatitis (NASH).
NASH causes the liver to swell and become damaged due to the fat deposits in the liver. NASH may get worse and may lead to serious liver scarring, called cirrhosis, and even liver cancer. This damage is like the damage caused by heavy alcohol use.
A move is currently underway to change the name nonalcoholic fatty liver disease to metabolic dysfunction-associated steatotic liver disease (MASLD). Experts also have recommended changing the name nonalcoholic steatohepatitis to metabolic dysfunction-associated steatohepatitis (MASH).
Products & Services
Symptoms
The liver
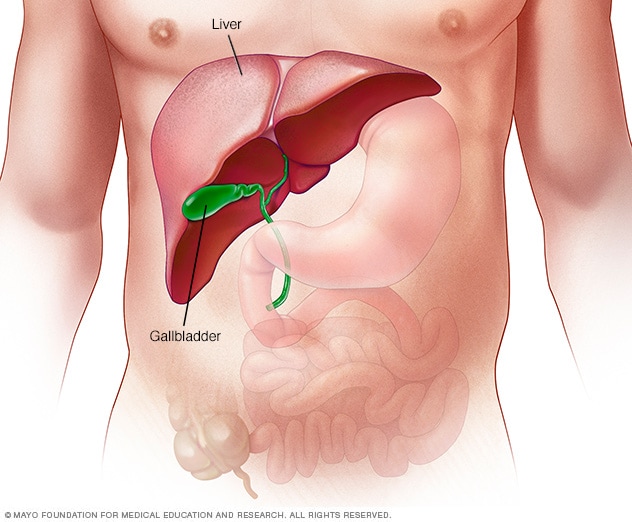
The liver
The liver is the largest internal organ in the body. It's about the size of a football. It sits mainly in the upper right portion of the stomach area, above the stomach.
NAFLD often has no symptoms. When it does, they may include:
- Fatigue.
- Not feeling well, or malaise.
- Pain or discomfort in the upper right belly area.
Possible symptoms of NASH and cirrhosis, or severe scarring, include:
- Itchy skin.
- Abdominal swelling, also called ascites (uh-SY-teez).
- Shortness of breath.
- Swelling of the legs.
- Spider-like blood vessels just beneath the skin's surface.
- Enlarged spleen.
- Red palms.
- Yellowing of the skin and eyes, or jaundice.
When to see a doctor
Make an appointment with a member of your health care team if you have lasting symptoms that worry you.
Causes
Experts don't know exactly why fat builds up in some livers and not others. They also don't fully understand why some fatty livers turn into NASH.
NAFLD and NASH are both linked to the following:
- Genetics.
- Overweight or obesity.
- Insulin resistance, which happens when your cells don't take up sugar in response to the hormone insulin.
- Type 2 diabetes, sometimes called high blood sugar or hyperglycemia.
- High levels of fats, especially triglycerides, in the blood.
These combined health problems may contribute to a fatty liver. However, some people get NAFLD even if they do not have any risk factors.
Risk factors
Many diseases and health problems can increase your risk of NAFLD, including:
- Family history of fatty liver disease or obesity.
- Growth hormone deficiency, which means the body doesn't make enough hormones to grow.
- High cholesterol.
- High levels of triglycerides in the blood.
- Insulin resistance.
- Metabolic syndrome.
- Obesity, especially when fat is centered in the waist.
- Polycystic ovary syndrome.
- Obstructive sleep apnea.
- Type 2 diabetes.
- Underactive thyroid, also called hypothyroidism.
- Underactive pituitary gland, or hypopituitarism.
NASH is more likely in these groups:
- People older than 50.
- People with certain genetic risk factors.
- People with obesity.
- People with diabetes or high blood sugar.
- People with symptoms of metabolic syndrome, such as high blood pressure, high triglycerides and a large waist size.
It is hard to tell apart NAFLD from NASH without a clinical evaluation and testing.
Complications
Healthy liver vs. liver cirrhosis
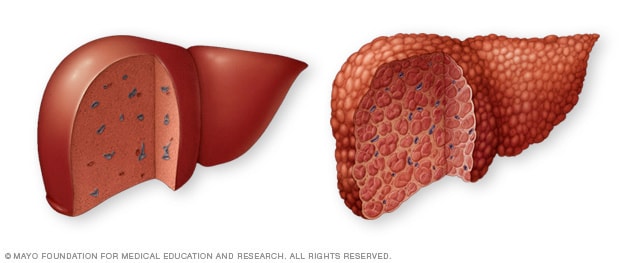
Healthy liver vs. liver cirrhosis
A healthy liver, at left, shows no signs of scarring. In cirrhosis, at right, scar tissue replaces healthy liver tissue.
Esophageal varices
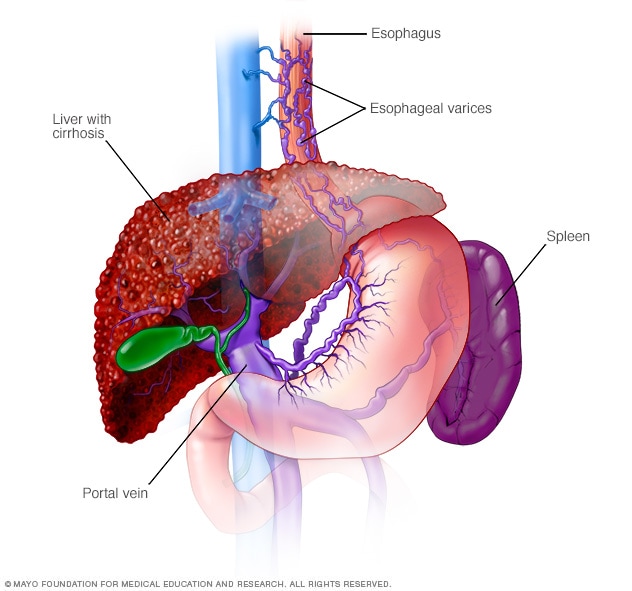
Esophageal varices
Esophageal varices are enlarged veins in the esophagus. They're often due to obstructed blood flow through the portal vein, which carries blood from the intestine to the liver.
Liver cancer
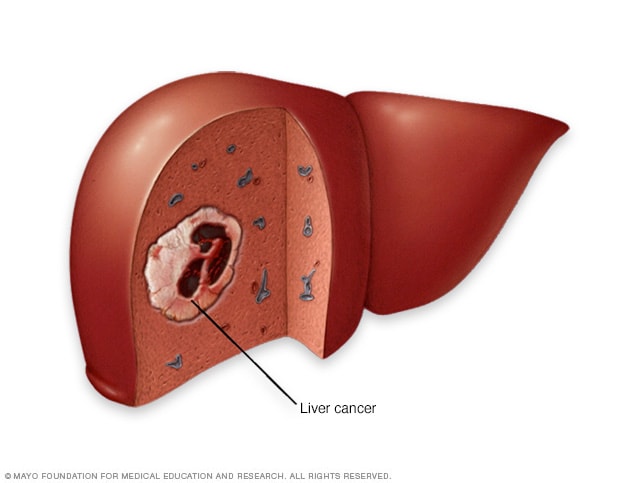
Liver cancer
Liver cancer begins in the liver cells. The most common type of liver cancer starts in cells called hepatocytes and is called hepatocellular carcinoma.
Severe liver scarring, or cirrhosis, is the main complication of NAFLD and NASH. Cirrhosis happens because of liver injury, such as the damage caused by inflammation in NASH. As the liver tries to stop inflammation, it creates areas of scarring, also called fibrosis. With ongoing inflammation, fibrosis spreads and takes up more liver tissue.
If nothing is done to stop the scarring, cirrhosis can lead to:
- Fluid buildup in the stomach area, called ascites.
- Swollen veins in your esophagus, or esophageal varices, which can rupture and bleed.
- Confusion, sleepiness and slurred speech, also called hepatic encephalopathy.
- Overactive spleen, or hypersplenism, which can cause too few blood platelets.
- Liver cancer.
- End-stage liver failure, which means the liver has stopped working.
Experts guess that about 24% of adults in the U.S. have NAFLD, and about 1.5% to 6.5% have NASH.
Prevention
To reduce your risk of NAFLD:
- Eat a healthy diet. Eat a healthy diet that's rich in fruits, vegetables, whole grains and healthy fats.
- Limit alcohol, simple sugars and portion sizes. Avoid sugary drinks like soda, sports drinks, juices and sweet tea. Drinking alcohol can damage your liver and should be avoided or minimized.
- Keep a healthy weight. If you are overweight or obese, work with your health care team to gradually lose weight. If you are a healthy weight, work to keep it by eating a healthy diet and exercising.
- Exercise. Be active most days of the week. Get an OK from your health care team first if you haven't been exercising regularly.