Diagnosis
Endoscopy
Endoscopy
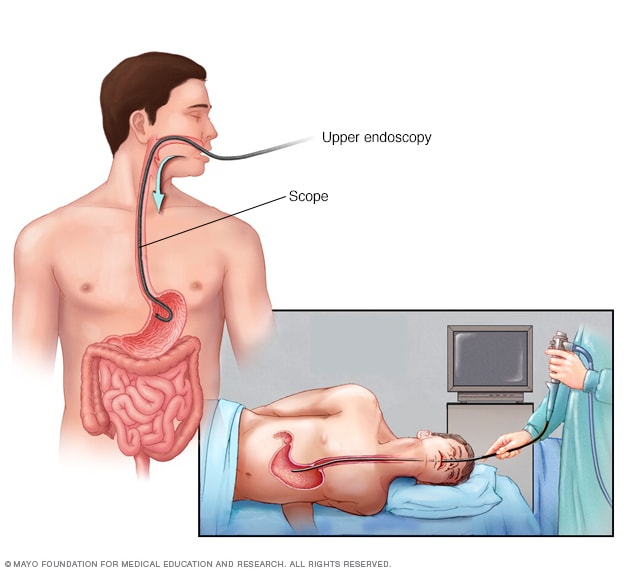
An endoscopy procedure involves inserting a long, flexible tube called an endoscope down your throat and into your esophagus. A tiny camera on the end of the endoscope allows views of your esophagus, stomach and the beginning of your small intestine, called the duodenum.
Your healthcare professional is likely to suspect gastritis after talking to you about your medical history and performing an exam. However, you also may have one or more of the following tests to find the exact cause.
-
Tests for H. pylori. Your healthcare professional may recommend tests such as a stool test or breath test to determine whether you have H. pylori. Which type of test you have depends on your situation.
For the breath test, you drink a small glass of clear, tasteless liquid that contains radioactive carbon. H. pylori germs break down the test liquid in your stomach. Later, you blow into a bag, which is then sealed. If you're infected with H. pylori, your breath sample will contain the radioactive carbon.
-
Passing a thin, flexible scope down the throat, called an endoscopy. Endoscopy is a procedure to examine the digestive system with a long, thin tube with a tiny camera, called an endoscope. The endoscope passes down the throat, into the esophagus, stomach and small intestine. Using the endoscope, your healthcare professional looks for signs of inflammation. Depending on your age and medical history, your healthcare professional may recommend this as a first test instead of testing for H. pylori.
If a suspicious area is found, your healthcare professional may remove small tissue samples, called a biopsy, to test in a lab. A biopsy also can identify the presence of H. pylori in your stomach lining.
- X-ray of your upper digestive system. X-rays can create images of your esophagus, stomach and small intestine to look for anything unusual. You may have to swallow a white, metallic liquid that contains barium. The liquid coats your digestive tract and makes an ulcer more visible. This procedure is called a barium swallow.
An endoscopy is a procedure used to visually examine your upper digestive system. During an endoscopy your doctor gently inserts a long, flexible tube, or endoscope, into your mouth, down your throat and into your esophagus. A fiber-optic endoscope has a light and tiny camera at the end.
Your doctor can use this device to view your esophagus, stomach and the beginning of your small intestine. The images are viewed on a video monitor in the exam room.
If your doctor sees anything unusual, such as polyps or cancer, he or she passes special surgical tools through the endoscope to remove tissue or collect a sample to examine it more closely.
Treatment
Treatment of gastritis depends on the specific cause. Acute gastritis caused by NSAIDs or alcohol may be relieved by stopping use of those substances.
Medicines used to treat gastritis include:
- Antibiotics to kill H. pylori. For H. pylori in your digestive tract, your healthcare professional may recommend a combination of antibiotics to kill the germs. Be sure to take the full antibiotic prescription, usually for 7 to 14 days. You also may take a medicine to block acid production. Once treated, your healthcare professional will retest you for H. pylori to be sure it has been destroyed.
-
Medicines that block acid production and promote healing. Medicines called proton pump inhibitors help reduce acid. They do this by blocking the action of the parts of cells that produce acid. You may get a prescription for proton pump inhibitors, or you can buy them without a prescription.
Long-term use of proton pump inhibitors, particularly at high doses, may increase your risk of hip, wrist and spine fractures. Ask your healthcare professional whether a calcium supplement may reduce this risk.
- Medicines to reduce acid production. Acid blockers, also called histamine blockers, reduce the amount of acid released into your digestive tract. Reducing acid relieves gastritis pain and encourages healing. You may get a prescription for an acid blocker, or you can buy one without a prescription.
- Medicines that neutralize stomach acid. Your healthcare professional may include an antacid in your treatment. Antacids neutralize existing stomach acid and can provide rapid pain relief. These help with immediate symptom relief but are generally not used as a primary treatment. Side effects of antacids can include constipation or diarrhea, depending on the main ingredients. Proton pump inhibitors and acid blockers are more effective and have fewer side effects.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
You may find some relief from symptoms if you:
- Don't drink alcohol. Alcohol can irritate the mucous lining of your stomach.
- Consider switching pain relievers. If you use pain relievers that increase your risk of gastritis, ask your healthcare professional whether acetaminophen (Tylenol, others) may be an option for you. This medicine is less likely to stir up your stomach problem.
Preparing for your appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
If your healthcare professional thinks that you might have gastritis, you may be referred to a doctor who specializes in digestive disorders, called a gastroenterologist.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you're experiencing, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down key personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements you're taking and the doses.
- Take a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For gastritis, some basic questions to ask include:
- What is likely causing my symptoms or condition?
- Should I be tested for H. pylori, or do I need an endoscopy?
- Could any of my medicines be causing my condition?
- What are other possible causes for my symptoms or condition?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What is the best course of action?
- What are alternatives to the primary approach you're suggesting?
- I have other health conditions. How can I best manage them together?
- Are there restrictions that I need to follow?
- Should I see a specialist?
- Is there a generic alternative to the medicine you're prescribing?
- Are there brochures or other printed material I can take? What websites do you recommend?
- What will determine whether I should schedule a follow-up visit?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- What are your symptoms?
- How severe are your symptoms? Would you describe your stomach pain as mildly uncomfortable or burning?
- Have your symptoms been continuous or occasional?
- Does anything, such as eating certain foods, seem to worsen your symptoms?
- Does anything, such as eating certain foods or taking antacids, seem to improve your symptoms?
- Do you experience any nausea or vomiting?
- Have you recently lost weight?
- How often do you take pain relievers, such as aspirin, ibuprofen or naproxen sodium?
- How often do you drink alcohol, and how much do you drink?
- How would you rate your stress level?
- Have you noticed any black stools or blood in your stool?
- Have you ever had an ulcer?
What you can do in the meantime
Before your appointment, avoid drinking alcohol and eating foods that seem to irritate your stomach. These foods may include those that are spicy, acidic, fried or fatty. But talk to your healthcare professional before stopping any prescription medicines you're taking.
Feb. 14, 2024