Diagnosis
Kidney biopsy
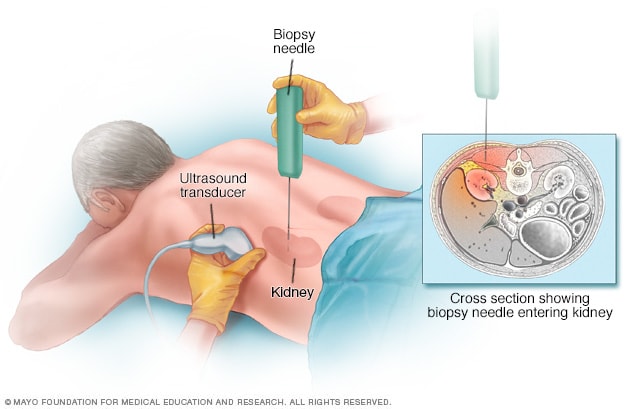
Kidney biopsy
During a kidney biopsy, a healthcare professional uses a needle to remove a small sample of kidney tissue for lab testing. The biopsy needle is put through the skin to the kidney. The procedure often uses an imaging device, such as an ultrasound transducer, to guide the needle.
Diabetic nephropathy usually is diagnosed during the regular testing that's part of managing diabetes. Get tested every year if you have type 2 diabetes or have had type 1 diabetes for more than five years.
Routine screening tests may include:
- Urinary albumin test. This test can detect a blood protein called albumin in urine. Typically, the kidneys don't filter albumin out of the blood. Too much albumin in your urine can mean that the kidneys aren't working well.
- Albumin/creatinine ratio. Creatinine is a chemical waste product that healthy kidneys filter out of the blood. The albumin/creatinine ratio measures how much albumin compared to creatinine is in a urine sample. It shows how well the kidneys are working.
- Glomerular filtration rate (GFR). The measure of creatinine in a blood sample may be used to see how quickly the kidneys filter blood. This is called the glomerular filtration rate. A low rate means the kidneys aren't working well.
Other diagnostic tests may include:
- Imaging tests. X-rays and ultrasound can show the makeup and size of the kidneys. CT and MRI scans can show how well blood is moving within the kidneys. You may need other imaging tests, as well.
- Kidney biopsy. This is a procedure to take a sample of kidney tissue to be studied in a lab. It involves a numbing medicine called a local anesthetic. A thin needle is used to remove small pieces of kidney tissue.
Mayo Clinic Health Letter & Books
Join thousands of readers who trust Mayo Clinic Health Letter for reliable health tips and insights. Start your journey to better health today.
Treatment
The first step in treating diabetic nephropathy is to treat and control diabetes and high blood pressure. Treatment includes diet, lifestyle changes, exercise and prescription medicines. Controlling blood sugar and blood pressure might prevent or delay kidney issues and other complications.
Medications
In the early stages of diabetic nephropathy, your treatment might include medicines to manage the following:
- Blood pressure. Medicines called angiotensin-converting enzyme (ACE) inhibitors and angiotensin 2 receptor blockers (ARBs) are used to treat high blood pressure.
-
Blood sugar. Medicines can help control high blood sugar in people with diabetic nephropathy. They include older diabetes medicines such as insulin. Newer drugs include Metformin (Fortamet, Glumetza, others), glucagon-like peptide 1 (GLP-1) receptor agonists and SGLT2 inhibitors.
Ask your health care professional if treatments such as SGLT2 inhibitors or GLP-1 receptor agonists might work for you. These treatments can protect the heart and kidneys from damage due to diabetes.
- High cholesterol. Cholesterol-lowering drugs called statins are used to treat high cholesterol and lower the amount of protein in urine.
- Kidney scarring. Finerenone (Kerendia) might help reduce tissue scarring in diabetic nephropathy. Research has shown that the medicine might lower the risk of kidney failure. It also may lower the risk of dying from heart disease, having heart attacks and needing to go to a hospital to treat heart failure in adults with chronic kidney disease linked to type 2 diabetes.
If you take these medicines, you'll need regular follow-up testing. The testing is done to see if your kidney disease is stable or getting worse.
Treatment for advanced diabetic nephropathy
Start your donor evaluation
Begin the process of becoming a living kidney or liver donor by clicking here to complete a health history questionnaire.
Kidney transplant
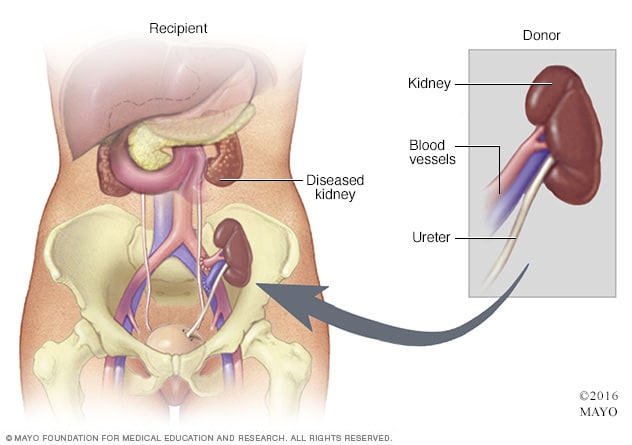
Kidney transplant
During kidney transplant surgery, the donor kidney is placed in your lower abdomen. Blood vessels of the new kidney are attached to blood vessels in the lower part of your abdomen, just above one of your legs. The new kidney's ureter is connected to your bladder. Unless they are causing complications, your own kidneys are left in place. Kidney transplant surgery usually lasts about 3 to 4 hours.
For kidney failure, also called end-stage kidney disease, treatment focuses on either replacing the work of your kidneys or making you more comfortable. Options include:
-
Kidney dialysis. This treatment removes waste products and extra fluid from the blood. Hemodialysis filters blood outside the body using a machine that does the work of the kidneys. For hemodialysis, you might need to visit a dialysis center about three times a week. Or you might have dialysis done at home by a trained caregiver. Each session takes 3 to 5 hours.
Peritoneal dialysis uses the inner lining of the abdomen, called the peritoneum, to filter waste. A cleansing fluid flows through a tube to the peritoneum. This treatment can be done at home or at work. But not everyone can use this method of dialysis.
- Transplant. Sometimes, a kidney transplant or a kidney-pancreas transplant is the best treatment choice for kidney failure. If you and your health care team decide on a transplant, you'll be assessed to find out if you can have the surgery.
- Symptom management. If you have kidney failure and you don't want dialysis or a kidney transplant, you'll likely live only a few months. Treatment may help keep you comfortable.
Potential future treatments
In the future, people with diabetic nephropathy may benefit from treatments being developed using techniques that help the body repair itself, called regenerative medicine. These techniques may help reverse or slow kidney damage.
For example, some researchers think that if a person's diabetes can be cured by a future treatment such as pancreas islet cell transplant or stem cell therapy, the kidneys might work better. These therapies, as well as new medicines, are still being studied.
Kidney Disease: How kidneys work, Hemodialysis, and Peritoneal dialysis
Lifestyle and home remedies
Diet, exercise and self-care are needed to control blood sugar and high blood pressure. Your diabetes care team can help you with the following goals:
- Monitor your blood sugar. Your health care team will tell you how often to check your blood sugar level to make sure you stay in your target range. You may, for example, need to check it once a day and before or after exercise. If you take insulin, you may need to check your blood sugar level several times a day.
- Be active most days of the week. Aim for at least 30 minutes or more of moderate to vigorous aerobic exercise on most days. Go for a total of at least 150 minutes a week. Activities might include brisk walking, swimming, biking or running.
- Eat a healthy diet. Eat a high-fiber diet with lots of fruits, nonstarchy vegetables, whole grains and legumes. Limit saturated fats, processed meats, sweets and salt.
- Quit smoking. If you smoke, talk with your health care professional about ways to quit.
- Stay at a healthy weight. If you need to lose weight, talk with your health care professional about ways to do so. For some people, weight-loss surgery is an option.
- Take a daily aspirin. Talk with your health care professional about whether you should take a daily low-dose aspirin to lower the risk of heart disease.
- Talk to your health care team. Make sure all your health care professionals know that you have diabetic nephropathy. They can take steps to protect your kidneys from more damage by not doing medical tests that use contrast dye. These include angiograms and computerized tomography (CT) scans.
Coping and support
If you have diabetic nephropathy, these steps may help you cope:
- Connect with other people who have diabetes and kidney disease. Ask a member of your health care team about support groups in your area. Or contact groups such as the American Association of Kidney Patients or the National Kidney Foundation for groups in your area.
- Stick to your usual routine, when possible. Try to keep your usual routine, doing the activities you enjoy and working, if your condition allows. This may help you cope with feelings of sadness or loss that you may have after your diagnosis.
- Talk with someone you trust. Living with diabetic nephropathy can be stressful, and it may help to talk about your feelings. You may have a friend or family member who is a good listener. Or you may find it helpful to talk with a faith leader or someone else you trust. Ask a member of your health care team for the name of a social worker or counselor.
Preparing for your appointment
Diabetic nephropathy most often is found during regular appointments for diabetes care. If you've been diagnosed with diabetic nephropathy recently, you may want to ask your health care professional the following questions:
- How well are my kidneys working now?
- How can I keep my condition from getting worse?
- What treatments do you suggest?
- How do these treatments change or fit into my diabetes treatment plan?
- How will we know if these treatments are working?
Questions for ongoing appointments
Before any appointment with a member of your diabetes treatment team, ask whether you need to follow any restrictions, such as fasting before taking a test. Questions to regularly review with your doctor or other members of the team include:
- How often should I check my blood sugar? What is my target range?
- What changes in my diet would help me better manage my blood sugar, cholesterol or blood pressure?
- When should I take my medicines? Do I take them with food?
- How does managing my diabetes affect treatment for other conditions I have? How can I manage my treatments better?
- When do I need to make a follow-up appointment?
- What should prompt me to call you or seek emergency care?
- Are there brochures or online sources you can suggest?
- Is there help for paying for diabetes supplies?
What to expect from your doctor
Your health care professional is likely to ask you questions during your appointments, including:
- Do you understand your treatment plan and know that you can follow it?
- How are you coping with diabetes?
- Have you had any low blood sugar?
- Do you know what to do if your blood sugar is too low or too high?
- What do you usually eat in a day?
- Are you exercising? If so, what type of exercise? How often?
- Do you sit a lot?
- What are you finding hard about managing your diabetes?
Oct. 24, 2023