Diagnosis
Upper endoscopy
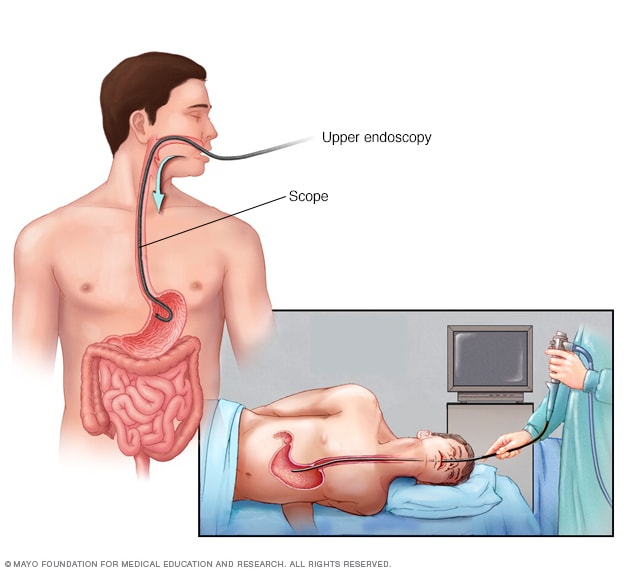
Upper endoscopy
An upper endoscopy procedure involves inserting a long, flexible tube called an endoscope down your throat and into your esophagus. A tiny camera on the end of the endoscope allows views of your esophagus, stomach and the beginning of your small intestine, called the duodenum.
Capsule endoscopy camera
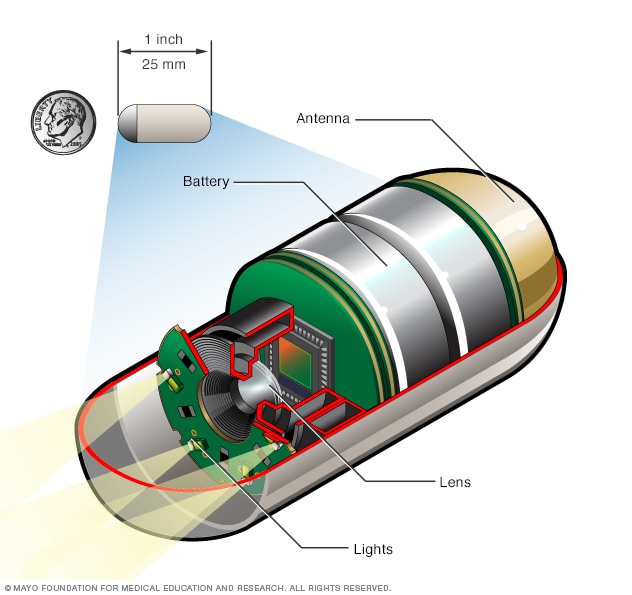
Capsule endoscopy camera
A capsule endoscopy procedure involves swallowing a tiny camera that's about the size of a large vitamin pill. The capsule contains lights to light up the digestive system, a camera to take images and an antenna that sends those images to a recorder worn on a belt.
Many people with celiac disease don't know they have it. Two blood tests can help diagnose it:
- Serology testing looks for antibodies in your blood. Elevated levels of certain antibody proteins indicate an immune reaction to gluten.
- Genetic testing for human leukocyte antigens (HLA-DQ2 and HLA-DQ8) can be used to rule out celiac disease.
It's important to be tested for celiac disease before trying a gluten-free diet. Eliminating gluten from your diet might make the results of blood tests appear in the standard range.
If the results of these tests indicate celiac disease, one of the following tests will likely be ordered:
- Endoscopy. This test uses a long tube with a tiny camera that's put into your mouth and passed down your throat. The camera enables the practitioner to view your small intestine and take a small tissue sample, called a biopsy, to analyze for damage to the villi.
- Capsule endoscopy. This test uses a tiny wireless camera to take pictures of your entire small intestine. The camera sits inside a vitamin-sized capsule, which you swallow. As the capsule travels through your digestive tract, the camera takes thousands of pictures that are transmitted to a recorder. This test is used in some situations where an exam of the entire or end of the small intestine is desired.
If you might have dermatitis herpetiformis, your health care professional may take a small sample of skin tissue to examine under a microscope.
If you're diagnosed with celiac disease, additional testing may be recommended to check your nutritional status. This includes levels of vitamins A, B-12, D and E, as well as mineral levels, hemoglobin and liver enzymes. Your bone health also may be checked with a bone density scan.
Treatment
A strict, lifelong gluten-free diet is the only way to manage celiac disease. Besides wheat, foods that contain gluten include:
- Barley.
- Bulgur.
- Durum.
- Farina.
- Graham flour.
- Malt.
- Rye.
- Semolina.
- Spelt (a form of wheat).
- Triticale.
A dietitian who works with people with celiac disease can help you plan a healthy gluten-free diet. Even trace amounts of gluten in your diet can be damaging, even if they don't cause symptoms.
Gluten can be hidden in foods, medicines and nonfood products, including:
- Modified food starch, preservatives and food stabilizers.
- Prescription and over-the-counter medications.
- Vitamin and mineral supplements.
- Herbal and nutritional supplements.
- Lipstick products.
- Toothpaste and mouthwash.
- Communion wafers.
- Envelope and stamp glue.
- Play dough.
- Certain makeup products.
Removing gluten from your diet will typically reduce inflammation in your small intestine, causing you to feel better and eventually heal. Children tend to heal more quickly than adults.
Vitamin and mineral supplements
If your anemia or nutritional deficiencies are severe, supplements may be recommended, including:
- Copper.
- Folic acid.
- Iron.
- Vitamin B-12.
- Vitamin D.
- Vitamin K.
- Zinc.
Vitamins and supplements are usually taken in pill form. If your digestive tract has trouble absorbing vitamins, you might be able to get them by injection.
Follow-up care
Medical follow-up at regular intervals can ensure that your symptoms have responded to a gluten-free diet. Your health care team may monitor your response with blood tests. Nutritional markers also are checked regularly.
For most people with celiac disease, eating a gluten-free diet allows the small intestine to heal. For children, that usually takes 3 to 6 months. For adults, complete healing might take several years.
If you continue to have symptoms or if symptoms recur, you might need an endoscopy with biopsies to determine whether your intestine has healed.
Medications to control intestinal inflammation
If your small intestine is severely damaged or you have refractory celiac disease, steroids may be recommended to control inflammation. Steroids can ease severe symptoms of celiac disease while the intestine heals.
Other drugs, such as azathioprine (Azasan, Imuran) or budesonide (Entocort EC, Uceris), might be used.
Treating dermatitis herpetiformis
If you have this skin rash, a medicine called dapsone may be recommended in addition to a gluten-free diet. Dapsone is taken by mouth. If you take dapsone, you'll need regular blood tests to check for side effects.
Refractory celiac disease
With refractory celiac disease, the small intestine doesn't heal. Refractory celiac disease can be quite serious, and there is currently no proven treatment. If you have refractory celiac disease, you may want to seek medical care at a specialized center.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
If you've been diagnosed with celiac disease, you'll need to avoid all foods that contain gluten. Ask your health care team for a referral to a dietitian, who can help you plan a healthy gluten-free diet.
Read labels
Avoid packaged foods unless they're labeled as gluten-free or have no gluten-containing ingredients, including emulsifiers and stabilizers that can contain gluten. In addition to cereals, pastas and baked goods, other packaged foods that can contain gluten include:
- Beers, lagers, ales and malt vinegars.
- Candies.
- Gravies.
- Imitation meats or seafood.
- Processed luncheon meats.
- Rice mixes.
- Salad dressings and sauces, including soy sauce.
- Seasoned snack foods, such as tortilla and potato chips.
- Seitan.
- Self-basting poultry.
- Soups.
Pure oats aren't harmful for most people with celiac disease, but oats can be contaminated by wheat during growing and processing. Ask your health care team if you can try eating small amounts of pure oat products.
Allowed foods
Many basic foods are allowed in a gluten-free diet, including:
- Eggs.
- Fresh meats, fish and poultry that aren't breaded, batter-coated or marinated.
- Fruits.
- Lentils.
- Most dairy products, unless they make your symptoms worse.
- Nuts.
- Potatoes.
- Vegetables.
- Wine and distilled liquors, ciders and spirits.
Grains and starches allowed in a gluten-free diet include:
- Amaranth.
- Buckwheat.
- Corn.
- Cornmeal.
- Gluten-free flours (rice, soy, corn, potato, bean).
- Pure corn tortillas.
- Quinoa.
- Rice.
- Tapioca.
- Wild rice.
Coping and support
It can be difficult, and stressful, to follow a completely gluten-free diet. Here are some ways to help you cope and to feel more in control.
- Get educated and teach family and friends. They can support your efforts in dealing with the disease.
- Follow your health care professional's recommendations. It's critical to eliminate all gluten from your diet.
- Find a support group. You might find comfort in sharing your struggles with people who face similar challenges. Organizations such as the Celiac Disease Foundation, Gluten Intolerance Group, the National Celiac Association and Beyond Celiac can help put you in touch with others who share your challenges.
Preparing for your appointment
You might be referred to a doctor who treats digestive diseases, called a gastroenterologist. Here's some information to help you prepare for your appointment.
What you can do
Until your appointment, continue eating your normal diet. Cutting gluten before you're tested for celiac disease can change the test results.
Make a list of:
- Your symptoms, including when they started and whether they've changed over time.
- Key personal information, including major stresses or recent life changes and whether anyone in your family has celiac disease or another autoimmune condition.
- All medications, vitamins or supplements you take, including doses.
- Questions to ask during your appointment.
For celiac disease, questions to ask include:
- What's the most likely cause of my symptoms?
- Is my condition temporary or long term?
- What tests do I need?
- What treatments can help?
- Do I need to follow a gluten-free diet?
Don't hesitate to ask other questions.
What to expect from your doctor
You may be asked the following questions:
- How severe are your symptoms?
- Have they been continuous or occasional?
- What, if anything, seems to improve your symptoms?
- What, if anything, seems to worsen your symptoms?
- What medications and pain relievers do you take?
- Have you been diagnosed with anemia or osteoporosis?
Sept. 12, 2023