Overview
Healthy shoulder joint
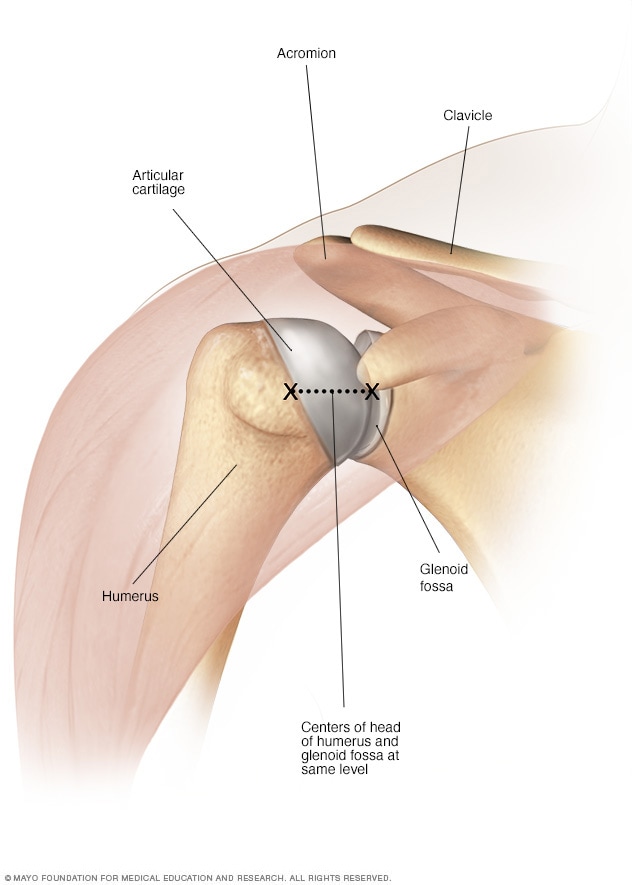
Healthy shoulder joint
In a healthy joint, the round head (ball) of the upper arm bone fits into a shallow socket in the shoulder.
Shoulder replacement removes damaged areas of bone and replaces them with parts made of metal and plastic (implants). This surgery is called shoulder arthroplasty (ARTH-row-plas-tee).
The shoulder is a ball-and-socket joint. The round head (ball) of the upper arm bone fits into a shallow socket in the shoulder. Damage to the joint can cause pain, weakness and stiffness.
Shoulder implants are available in a few different shapes and a range of sizes. Replacement options include partial and total using either anatomic or reverse implants.
Why it's done
Anatomic total shoulder replacement
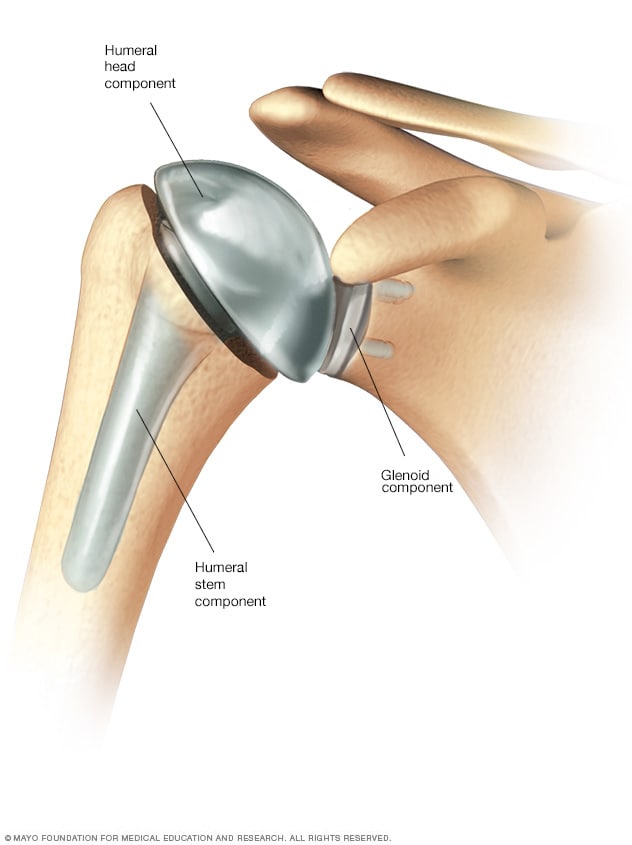
Anatomic total shoulder replacement
In an anatomic total shoulder replacement, the ball and the socket are replaced with implants that resemble the natural shape of the bones.
Reverse total shoulder replacement
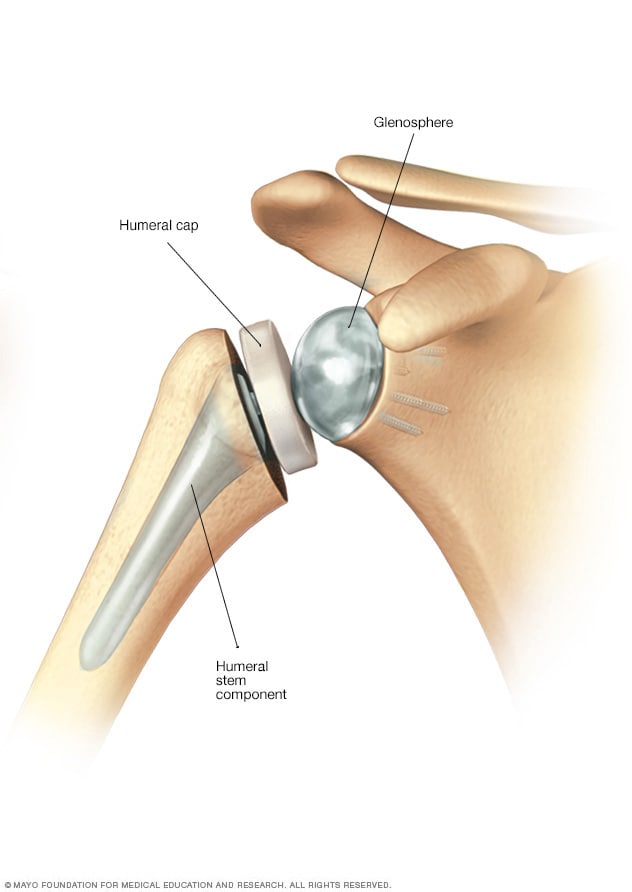
Reverse total shoulder replacement
In a reverse total shoulder replacement, the ball implant is attached to the shoulder blade and the socket is attached to the upper arm bone.
Shoulder replacement surgery is done to relieve pain and other symptoms that result from damage to the shoulder joint.
Conditions that can damage the joint include:
- Osteoarthritis. Known as wear-and-tear arthritis, osteoarthritis damages the cartilage that covers the ends of bones and helps joints move smoothly.
- Rotator cuff injuries. The rotator cuff is a group of muscles and tendons that surround the shoulder joint. Rotator cuff injuries sometimes can result in damage to cartilage and bone in the shoulder joint.
- Fractures. Fractures of the upper end of the humerus may require replacement, either as a result of the injury or when the prior surgery for fracture fixation has failed.
- Rheumatoid arthritis and other inflammatory disorders. Caused by an overactive immune system, the inflammation associated with rheumatoid arthritis can damage the cartilage and occasionally the underlying bone in the joint.
- Osteonecrosis. Some types of shoulder conditions can affect blood flow to the humerus. When a bone is starved of blood, it can collapse.
Shoulder replacement procedures
Depending on the type of joint damage you have, your doctor may recommend one of the following shoulder replacement options:
- Anatomic total shoulder replacement. Both the ball and the socket are replaced. The implants resemble the natural shape of the bones.
- Reverse total shoulder replacement. Both the ball and the socket are replaced, but the implants are reversed. The ball is attached to the shoulder blade and the socket is attached to the upper arm bone. This option typically is preferred if the rotator cuff is severely damaged.
- Partial shoulder replacement. Only the head (ball) of the joint is replaced. It may be recommended when only the ball side of the joint is damaged.
Total shoulder replacement options
Reverse shoulder replacement may be a better way to improve the joints function and reduce pain, especially if the joint is affected by arthritis. This operation is also called reverse arthroplasty. Artho means joint. Plasty means to mold surgically.
The top of the arm bone fits into a socket on the shoulder blade. In a typical shoulder replacement, a plastic lining is attached to the socket to allow smooth movement. The surgeon removes the top of the arm bone and inserts a metal stem with a ball on the end. However, if the rotator cuff is severely damaged, the joint may not be stable or work properly.
In a reverse shoulder replacement, the normal ball and socket structure is reversed. An artificial ball is attached to the shoulder blade. An artificial socket is attached to the top of the arm bone. The large deltoid muscle that covers the shoulder is typically able to move the arm.
Partial shoulder replacement
In some people, the top of the arm bone needs to be replaced, but the socket is still in good shape. In others, the bone in the socket is too worn out and not strong enough to hold a new lining. In these cases an operation called a hemiarthroplasty may be the best option. Hemi means partial.
As seen before, the surgeon exposes the joint, prepares the top of the arm bone and inserts a metal stem with a ball on the end. If the socket is worn out, the surgeon smooths and reshapes it. The arm bone is then put back in place.
Risks
Although rare, it's possible that shoulder replacement surgery won't lessen your pain or make it go away completely. The surgery may not fully restore the movement or strength of the joint. In some cases, another surgery may be needed.
Potential complications of shoulder replacement surgery include:
- Dislocation. It's possible for the ball of your new joint to come out of the socket.
- Fracture. The humerus bone, the scapula or the glenoid bone can break during or after surgery.
- Implant loosening. Shoulder replacement components are durable, but they may loosen or become worn over time. In some cases, you may need another surgery to replace the loose components.
- Rotator cuff failure. The group of muscles and tendons that surround the shoulder joint (the rotator cuff) occasionally wear out after a partial or total anatomic shoulder replacement.
- Nerve damage. Nerves in the area where the implant is placed can be injured. Nerve damage can cause numbness, weakness and pain.
- Blood clots. Clots can form in the veins of the leg or arm after surgery. This can be dangerous because a piece of a clot can break off and travel to the lung, the heart or, rarely, the brain.
- Infection. Infection can occur at the incision site or in the deeper tissue. Surgery is sometimes needed to treat it.
How you prepare
More information
Outpatient joint replacement: Is it a safe option?
Before surgery is scheduled, you'll meet with your surgeon for evaluation. This visit typically includes:
- A review of your symptoms
- A physical exam
- X-rays and computerized tomography (CT) of your shoulder
Some questions you may want to ask include:
- What type of surgery do you recommend?
- How will my pain be managed after surgery?
- How long will I have to wear a sling?
- What kind of physical therapy will I need?
- How will my activities be restricted after surgery?
- Will I need to have someone help me at home for a while?
Other members of the care team will assess your readiness for surgery. You'll be asked about your medical history, your medicines and whether you use tobacco. Tobacco interferes with healing.
You may meet with a physical therapist who will explain how to do physical therapy exercises and how to use a type of sling (immobilizer) that prevents your shoulder from moving.
Currently, many people leave the hospital the same day of the shoulder replacement procedure.
What you can expect
Before the procedure
Follow your surgeon's directions about bathing, eating and taking medicines the day before and the day of surgery.
During the procedure
A team member will talk with you about how you'll be sedated for surgery. Most people get general anesthesia and a nerve block. General anesthesia puts you into a deep sleep. The nerve block numbs your shoulder so that pain control can continue after you wake up from general anesthesia. The surgery usually takes 1 to 2 hours.
After the procedure
After surgery, you'll rest in a recovery area for a short time. X-rays will be obtained. Your shoulder will be in an immobilizer. Don't try to move your shoulder unless you're told to do so.
How long you stay after surgery depends on your individual needs. Many people can go home that same day.
Your shoulder replacement surgery at Mayo Clinic
If you're planning to have shoulder replacement surgery at Mayo Clinic, the following resources will explain what to expect and how to prepare.
Results
After shoulder replacement, most people have less pain than they did before surgery. Many have no pain. Most people also have improved range of motion and strength.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feb. 02, 2024