Overview
Female reproductive system
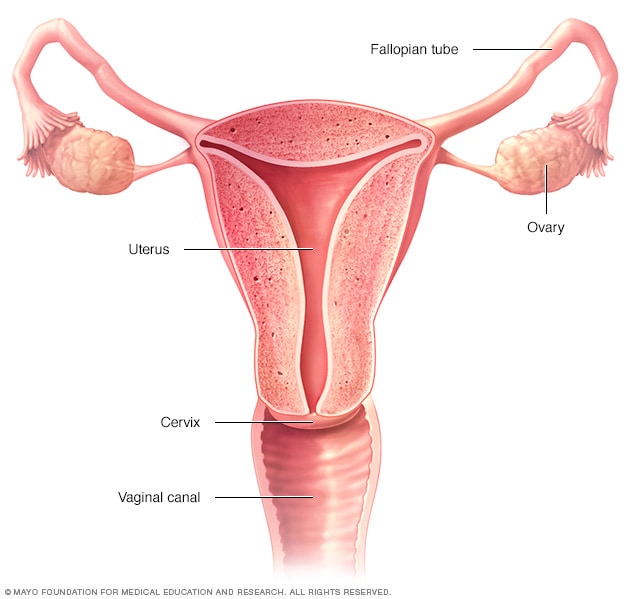
Female reproductive system
The ovaries, fallopian tubes, uterus, cervix and vagina, also called the vaginal canal, make up the female reproductive system.
An oophorectomy is surgery to remove one or both of the ovaries. The ovaries are almond-shaped organs that sit on each side of the uterus in the pelvis. The ovaries contain eggs and produce hormones that control the menstrual cycle.
When an oophorectomy (oh-of-uh-REK-tuh-me) involves removing both ovaries, it's called bilateral oophorectomy. When the surgery involves removing only one ovary, it's called unilateral oophorectomy. Sometimes surgery to remove the ovaries also involves removing the nearby fallopian tubes. This procedure is called a salpingo-oophorectomy.
An oophorectomy can be done as part of a hysterectomy, which is an operation to remove the uterus. Not every hysterectomy procedure involves removing the ovaries.
Why it's done
Ovarian cancer
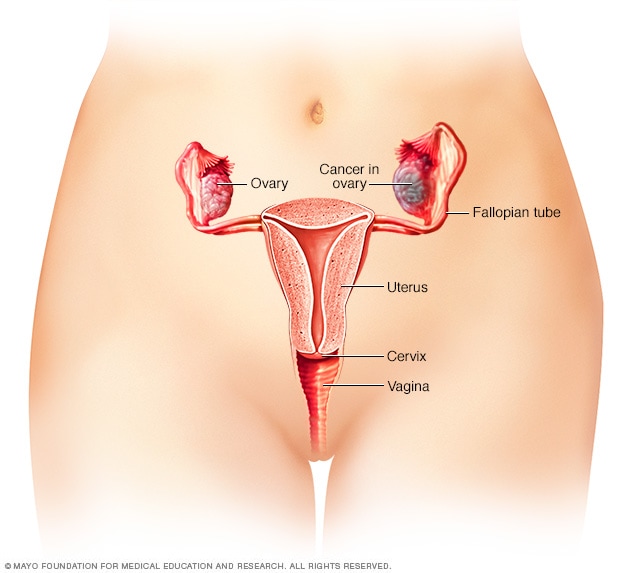
Ovarian cancer
Ovarian cancer is a type of cancer that begins in the ovaries. The ovaries are each about the size of an almond. They produce eggs, called ova, as well as the hormones estrogen and progesterone.
An oophorectomy may be done to treat or prevent certain health issues. It may be used for:
- A tubo-ovarian abscess. A tubo-ovarian abscess is a pus-filled pocket involving a fallopian tube and an ovary.
- Endometriosis. Endometriosis happens when tissue similar to the uterus lining grows outside of the uterus. It can cause cysts to form on the ovaries, called endometriomas.
- Noncancerous ovarian tumors or cysts. Small tumors or cysts may form on the ovaries. Cysts may burst and cause pain and other problems. Removing the ovaries can prevent this.
- Ovarian cancer. Oophorectomy may be used to treat ovarian cancer.
- Ovarian torsion. Ovarian torsion happens when an ovary becomes twisted.
- Reducing cancer risk. Oophorectomy may be used in people who have a high risk of ovarian cancer or breast cancer. Oophorectomy lowers the risk of both kinds of cancer. Research shows that some ovarian cancers start in the fallopian tubes. Because of this, the fallopian tubes may be removed during an oophorectomy that's done to lower the risk of cancer. A procedure that removes the ovaries and the fallopian tubes is called a salpingo-oophorectomy.
Risks
An oophorectomy is a fairly safe procedure. However, with any surgical procedure, there are risks involved.
Risks of an oophorectomy include the following:
- Bleeding.
- Damage to nearby organs.
- Inability to get pregnant without medical help if both ovaries are removed.
- Infection.
- Remaining ovary cells that continue to cause period symptoms, such as pelvic pain. This is called ovarian remnant syndrome.
- Rupture of a growth during surgery. If the growth is cancerous, this could spill cancer cells in the belly where they might grow.
Menopause after oophorectomy
If you have periods they will stop if both ovaries are removed. This is called menopause. It happens because your body is no longer getting the hormones made in the ovaries. These hormones include estrogen and progesterone. A sudden loss in this source of hormones can cause complications such as:
- Menopause symptoms, such as hot flashes and vaginal dryness.
- Depression or anxiety.
- Heart disease.
- Memory problems.
- Decreased sex drive.
- Decreased bone density, called osteoporosis.
Having an oophorectomy at a younger age, such as before 45, may increase the risks related to early menopause. Talk with your healthcare team about the risks related to your situation.
Taking low doses of hormone replacement medicines after surgery and until about age 50 may reduce the risk of these complications. But hormone replacement therapy has risks of its own. Talk about your options with your healthcare team.
How you prepare
To prepare for an oophorectomy, you may be asked to:
- Tell your healthcare team about any medicines, vitamins or supplements you're taking. Some substances could interfere with the surgery.
- Stop taking aspirin or other blood-thinning medicines. If you take blood thinners, your healthcare team will tell you when to stop taking these medicines. Sometimes a different blood-thinning medicine is given around the time of surgery.
- Stop eating before surgery. You'll receive specific instructions from your healthcare team about eating. You may need to stop eating several hours before surgery. You may be given the OK to drink liquids up to a certain time before surgery. Follow the instructions from your healthcare team.
- Have testing done. Testing may be needed to help the surgeon plan for the procedure. Imaging tests, such as an ultrasound, may be used. A blood test also may be needed.
Plan for infertility
After oophorectomy you may need medical help to become pregnant. If you want to have children, talk with your healthcare team about how your surgery may impact your plans. There may still be ways to become pregnant, depending on your situation. Ask your healthcare professional to refer you to a fertility specialist who can review your options with you.
What you can expect
Before oophorectomy
A member of your healthcare team will tell you when and where to arrive for your oophorectomy. If other preparation is needed, you may start in one area and move to another area for surgery. The surgery is often done as an outpatient procedure. Most people go home on the same day.
During oophorectomy
Laparoscopic oophorectomy
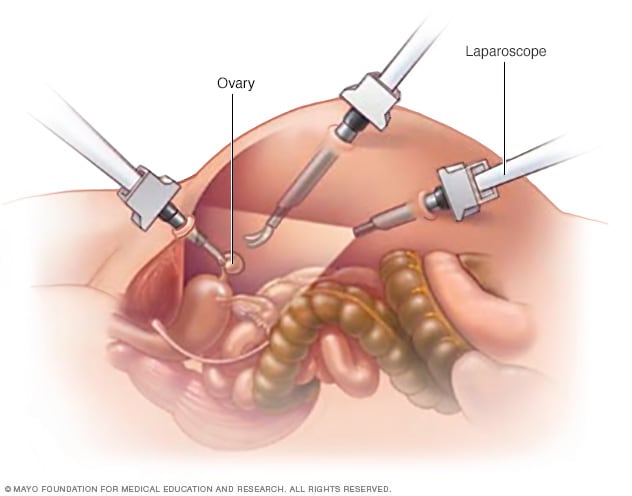
Laparoscopic oophorectomy
Laparoscopic oophorectomy uses special tools inserted through multiple incisions in the abdomen to remove the ovaries.
An oophorectomy is usually performed under general anesthesia, so you're in a sleep-like state during the surgery. To access the ovaries, the surgeon makes an incision in the abdomen.
Where the incision is placed depends on what type of surgery you're having and the reason for the surgery. Sometimes oophorectomy surgery uses one longer incision. This type of surgery is sometimes called open surgery or a laparotomy.
Sometimes the surgeon makes a few small incisions in the abdomen to get to the ovaries. Special tools go through the incisions to perform the procedure. This includes a tiny camera that transmits video that the surgeon uses to guide the tools. This type of surgery is sometimes called a minimally invasive surgery or laparoscopic surgery. Minimally invasive surgery also can be done with the help of a surgical robot. During minimally invasive robotic surgery, the surgeon sits at a console and uses controllers to operate the tools.
The type of surgery your surgeon uses depends on your situation. People who have minimally invasive surgery tend to recover more quickly. They may have less pain and spend less time in the hospital. But minimally invasive surgery isn't right for everyone. Sometimes the surgery starts out as minimally invasive surgery but needs to switch to an open procedure.
Once the incision or incisions are made in the abdomen, the surgeon works to remove the ovaries. One or both ovaries are separated from the blood supply and surrounding tissue. They are then taken out of your abdomen through the incision. The fallopian tubes or uterus may be removed at this time if that is part of the surgical plan.
As the surgery is completed, the incision is closed with stitches. Often these stitches are the type that dissolve over time.
After oophorectomy
After an oophorectomy, you can expect to:
- Spend time in a recovery room as your anesthesia wears off.
- Move to a hospital room where you may continue recovering.
- Get up and about as soon as you're able to help your recovery.
Most people can go home after oophorectomy surgery and won't need to spend the night in the hospital.
Results
How quickly you can go back to your daily activities after an oophorectomy depends on your situation. Factors may include the reason for your surgery and how it was performed.
Most people can return to full activity in 2 to 4 weeks after surgery. Talk with your healthcare team about what to expect.