Jan. 18, 2019
Mayo Clinic is pioneering advances in fetal surgery, allowing for earlier intervention to manage congenital anomalies. Although rare, these anomalies — including pulmonary hypoplasia in congenital diaphragmatic hernia (CDH) and fetal lower urinary tract obstruction (LUTO) — carry significant risk of mortality and disability.
"Typically, these problems have been treated after birth. But we are committed to developing surgical methods to reverse these conditions in utero and improve fetal development," says Rodrigo Ruano, M.D., Ph.D., chair of Maternal and Fetal Medicine at Mayo Clinic in Rochester, Minnesota.
Fetal surgery requires a multidisciplinary team with specialists in maternal-fetal medicine, pediatric surgery, neonatology, radiology and anesthesiology, as well as pediatric otolaryngology, nephrology, urology and neurosurgery, as needed. As a major tertiary medical center, Mayo Clinic Children's Center has the expertise to manage these complex patients, including providing both maternal and pediatric anesthesia. "We also work to establish collaborative relationships, so we can share care with the patient's home physician," Dr. Ruano says.
Novel therapy for CDH
Novel fetal surgery for congenital diaphragmatic hernia
Novel fetal surgery for congenital diaphragmatic hernia
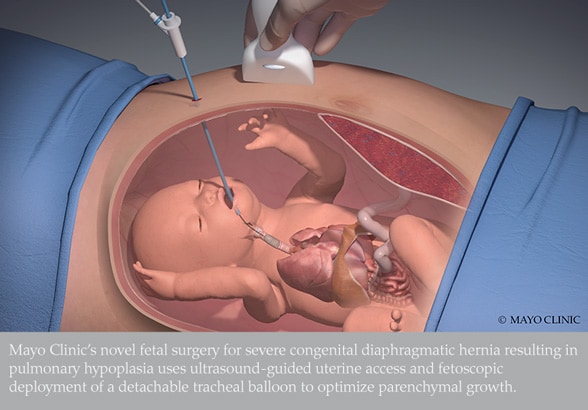
Mayo Clinic's novel fetal surgery for severe congenital diaphragmatic hernia resulting in pulmonary hypoplasia uses ultrasound-guided uterine access and fetoscopic deployment of a detachable tracheal balloon to optimize parenchymal growth.
Mayo Clinic has demonstrated the feasibility and safety of fetal endoscopic tracheal occlusion for severe CDH resulting in pulmonary hypoplasia, a life-threatening anomaly. The novel procedure is performed percutaneously with ultrasound-guided uterine access and fetoscopic deployment of a detachable tracheal balloon at 26 to 30 weeks of gestation. The balloon is intended to remain in place until about 34 weeks of gestation, when it is removed, preferentially through a fetoscopic procedure. The treatment optimizes parenchymal growth, improving pulmonary hypoplasia and vascular remodeling.
In the June 2018 edition of Mayo Clinic Proceedings, a specialized multidisciplinary group including Dr. Ruano described significant improvement after the procedure in two recent cases: Lung growth essentially doubled in one fetus and increased by one-third in the other. After birth, when the infants left the hospital, the first was breathing normally and the second required minimal nasal cannula oxygen support.
"Our experience indicates that fetuses with severe CDH have higher survival rates when treated prenatally, and Mayo Clinic has established a successful multidisciplinary fetoscopic tracheal occlusion program," Dr. Ruano says. "Although we have seen the beneficial effects of the tracheal balloon, we don't yet understand the mechanism for lung regrowth as part of in utero regenerative medicine. Our research on the regenerative principles of the lungs continues."
Prenatal management of LUTO
Mayo Clinic Children's Center is one of the few centers with a multidisciplinary program to treat LUTO prenatally. Depending on the nature of the blockage, treatment might consist of cystoscopy, vesicoamniotic shunting or operative cystoscopy. The shunting procedure entails the placement of a shunt in the fetal bladder to allow urine to flow from the bladder to the amniotic cavity; the shunt remains in place until birth.
Dr. Ruano participated in a study that reported a survival rate of 86 percent for fetuses with LUTO who had prenatal intervention; about two-thirds of the surviving infants had normal renal function at six-month follow-up. "Without prenatal treatment, the outlook for fetuses with LUTO is very poor. But we have lacked a standardized classification of LUTO to guide prenatal intervention," Dr. Ruano says.
Dr. Ruano developed a prenatal evaluation that estimates renal function by combining urinary biochemistry profiles and the ultrasound characteristics of fetal kidneys. When indicated, prenatal intervention occurs as early as possible after the LUTO diagnosis, often within two days. For children born with compromised renal function, the Mayo Clinic Children's Center can provide care after birth, including surgical correction of LUTO, renal monitoring, and dialysis or kidney transplant.
"We care for the whole patient throughout the patient's life, starting before birth," Dr. Ruano says. "Mayo Clinic is committed to advancing care in this area."
For more information
Ruano R, et al. Fetoscopic therapy for severe pulmonary hypoplasia in congenital diaphragmatic hernia: A first in prenatal regenerative medicine at Mayo Clinic. Mayo Clinic Proceedings. 2018;93:693.