July 11, 2023
Physicians and their patients can confidently choose treatment with minimally invasive surgery for high-risk endometrial cancer, according to study findings published in the January 2023 issue of Obstetrics & Gynecology. The study found that disease-free and overall survival were the same regardless of a minimally invasive or open surgical approach used for hysterectomy to treat this aggressive cancer. Both are oncologically and surgically safe.
"This reassures the medical community that using minimally invasive surgery for high-risk cancer is the right approach. It reinforces the fact that this type of surgery is important for endometrial cancer, and I would recommend it for patients with high-risk tumors."
Though other researchers previously had conducted studies on this topic, study participants were mostly those with low-risk endometrial cancer, such as the participants in a study published in a 2017 of JAMA. Also, the studies were largely retrospective. The majority of published studies on this topic did not include enough high-risk endometrial cancers to determine whether minimally invasive and open surgical approaches had equivalent oncologic outcomes. A far lower incidence of this aggressive cancer — than other endometrial cancers — likely impacted the lack of data on this tumor type, according to the Obstetrics & Gynecology publication.
To answer the question for high-risk endometrial cancer of whether both surgical approaches and corresponding outcomes were equivalent, or one method was superior, Dr. Mariani and colleagues conducted their study. They sought to give physicians — and their patients with this type of cancer — answers to empower educated surgical decision-making.
Highlights of study design and findings
The investigators designed the study with the help of M. Hassan Murad, M.D., a preventive medicine specialist and expert in systematic review and meta-analysis at Mayo Clinic in Minnesota. The study design combined a cohort study of 542 patients with high-risk endometrial cancer and a systematic literature review including 2,332 patients with high-risk endometrial cancer from 14 different studies. The investigators used a random-effects model for a meta-analysis that combined the retrospective cohort of Mayo Clinic patients with those from published studies.
Disease-free and overall survival did not differ with any statistical significance between women who had minimally invasive surgery and those who had open abdominal surgery, according to the meta-analysis.
The investigators then performed a subgroup analysis by early- or advanced-stage endometrial cancer. Again, no differences in outcomes appeared by surgical type.
Benefits of findings for physicians and their patients
Dr. Mariani says that as minimally invasive surgery for high-risk endometrial cancer has equivalent oncologic outcomes to open surgery, it also can benefit patients in ways such as:
- Better aesthetics. This surgical approach allows patients a better aesthetic with only a small scar on the abdomen versus a larger incision for open surgery.
- Faster healing. A smaller incision enables faster healing than a large, open incision. More rapid healing also allows the patient to move to the next stage of treatment faster, if applicable.
- Quicker return to home. Patients who have robotic surgery, a type of minimally invasive surgery, go home on the same day as the surgery.
- Lower risk with elevated BMI. Dr. Mariani notes that patients with high-risk endometrial cancer often have high BMI. Making a large incision in the abdomen with open surgery is riskier for these patients than having a small incision.
- Decreased infection risk. Infection risk with minimally invasive surgery is lower than with open surgery.
The decision to refer or keep the patient at home
Sentinel lymph nodes at Mayo Clinic
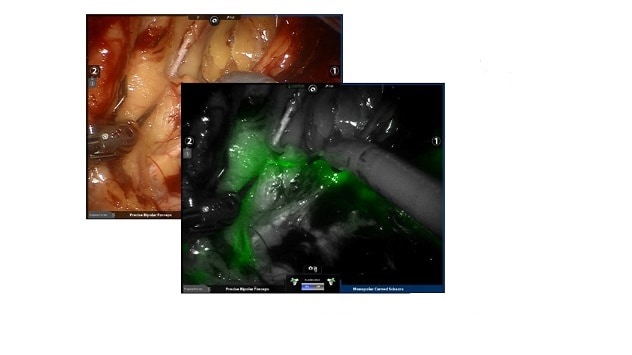
Sentinel lymph nodes at Mayo Clinic
A minimally invasive hysterectomy plus staging, first line therapy for endometrial cancer, is not a complex surgery, but it requires a gynecologic oncologist, according to Dr. Mariani. He indicates that surgeons in the community can perform this surgery successfully only if they have training in minimally invasive surgery and can perform a sentinel lymph node biopsy.
However, referral to a quaternary care center such as Mayo Clinic may be the best pathway for a patient with high-risk endometrial cancer who may need adjuvant therapy and access to appropriate clinical trials, says Dr. Mariani.
About high-risk endometrial cancer
Among gynecologic cancers, endometrial cancer is the most prevalent, says Dr. Mariani. High-risk endometrial cancer such as clear cell carcinoma and uterine serous papillary carcinoma account for only 10% to 15% of all endometrial cancer, but they account for 40% to 50% of all endometrial cancer-related mortality, according to a 2003 publication in International Journal of Radiation Oncology*Biology*Physics and a 1996 publication in Clinical Obstetrics and Gynecology. High-risk endometrial cancer involves a tumor that is biologically more aggressive, says Dr. Mariani. The International Federation of Gynecology and Obstetrics defines high-risk histology as meeting the following criteria: grade 3 endometrioid, serous, clear cell, mixed histology or uterine carcinosarcoma.
Dr. Mariani indicates that a gynecologic oncologist may suspect a high-risk tumor following pre-surgical imaging. A biopsy, which the surgeon performs prior to full surgery, can indicate high-risk status under a microscope in pathology, telling the surgeon to expect aggressive disease.
"For the pathologist and the molecular biologist, high-risk endometrial cancer and lower risk endometrial cancer look different," says Dr. Mariani.
High-risk endometrial tumors are disorganized and "kind of a mess genomically," with significant DNA changes, he says.
Of patients diagnosed with endometrial cancer, 1 out of 4 will have a high-risk tumor, says Dr. Mariani. He calls this "reasonably common," indicating that gynecologic surgeons at Mayo Clinic in Minnesota see about 100 patients in the high-risk category yearly. Most women he sees with this type of cancer are beyond childbearing years, with the vast majority around age 65.
There are four molecular categories of endometrial cancer, says Dr. Mariani, including the following:
- Mutation in DNA polymerase epsilon, called POLE, ultramutated or indolent.
- No specific molecular subtype.
- Copy number low.
- Copy number high, considered high-risk.
More than 95% of patients with endometrial cancer have hysterectomy first as standard therapy, says Dr. Mariani. Sometimes the gynecologic oncologist will send a patient to radiation therapy, often involving vaginal brachytherapy, 6 to 9 weeks post-surgically. If the patient has lymph node metastases, the patient will then have external beam radiation. Those at high risk of recurrence post-surgically have chemotherapy.
For your information
Dinoi G, et al. Minimally invasive compared with open surgery in high-risk endometrial cancer: A systematic review and meta-analysis. Obstetrics & Gynecology. 2023;141:59.
Janda M, et al. Effect of total laparoscopic hysterectomy vs total abdominal hysterectomy on disease-free survival among women with stage I endometrial cancer: A randomized clinical trial. JAMA. 2017;317:1224.
Murphy KT, et al. Outcome and patterns of failure in pathologic stages I–IV clear-cell carcinoma of the endometrium: Implications for adjuvant radiation therapy. International Journal of Radiation Oncology*Biology*Physics. 2003;55:1272.
Nicklin JL, et al. Endometrial papillary serous carcinoma: Patterns of spread and treatment. Clinical Obstetrics and Gynecology. 1996;39:686.
Refer a patient to Mayo Clinic.