May 19, 2018
Perioperative and postoperative MRI of hemangioblastoma
Perioperative and postoperative MRI of hemangioblastoma
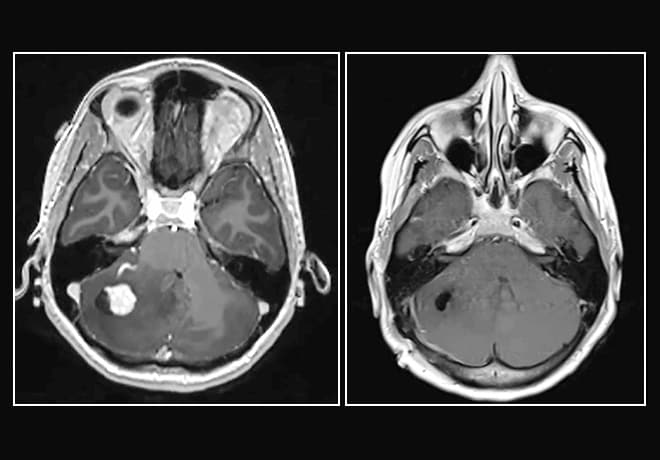
On the left, preoperative MRI of a hemangioblastoma shows significant swelling. On the right, MRI shows complete removal of the lesion after minimally invasive surgery.
Mayo Clinic offers minimally invasive surgery using a tubular retractor system that substantially lowers the risk of damaging eloquent tissue during removal of deep-seated lesions. The procedure can be an option for selected patients with subcortical high-grade glioma, metastatic brain tumors or vascular lesions.
"It's a stealth approach. You go deep within the brain, you cause minimal disturbance — it's like no one knew you were there," says Kaisorn L. Chaichana, M.D., a neurosurgeon at Mayo Clinic in Jacksonville, Florida. "Patients also have less blood loss and recover much faster than they do with open surgery."
The typical approach to deep-seated lesions — involving large craniotomies, extensive cortical and subcortical dissection, and retractor blades — can be associated with significant morbidity. "One advantage of our keyhole procedure is that the incision can be just 1.5 to 2 inches long," Dr. Chaichana says. "The bone opening is a little bit larger than a silver dollar, and we work through a tube with a diameter that's a little bit smaller than a dime."
The tubular retractor splays the brain's white matter tracts, exposing the tumor surface and providing a small working channel for lesion dissection and removal. "Bladed retractors stretch the white matter tracts and often sever them. The tubular retractor pushes the tracts aside, and the tracts go back into place when you pull out the tube," Dr. Chaichana says.
The minimally invasive procedure also uses exoscopic visualization, which provides greater magnification than microscope technology. "The exoscope is very ergonomic for the surgeon and allows us to get light down into areas where we couldn't before," Dr. Chaichana says.
Depending on the lesion's location, the minimally invasive surgery takes about 2.5 hours. Patients generally go home on the second postoperative day. "Typically, patients who have open resection stay in the hospital for five or six days and often need rehabilitation," Dr. Chaichana notes.
Tubular retraction can also be an effective tool for diagnosing deep-seated lesions, to guide adjuvant therapy when extensive surgical resection isn't appropriate. In a study published in the November 2017 issue of the Journal of Neurological Surgery Part A: Central European Neurosurgery, Dr. Chaichana and colleagues reported that a tubular retractor system with exoscopic visualization can safely access deep-seated lesions to provide adequate tissue for diagnosis and molecular evaluation.
The researchers noted that tubular retraction yields more tissue than stereotactic needle biopsy and provides enhanced visualization. "You can see the pathology up close. You know exactly what tissue you're getting," Dr. Chaichana says.
These minimally invasive techniques require a high level of expertise. "This procedure is technique heavy. Surgeons who typically do this must be skilled in minimally invasive surgery, endoscopic as well as exoscopic," Dr. Chaichana says.
In addition to skilled neurosurgeons, the procedure requires subspecialized expertise in neuroimaging. "You need a high-quality neuroradiology team that's able to identify the location of white matter tracts and to monitor them," Dr. Chaichana says.
"This surgery is done on the highest-risk patients," he adds. "At Mayo Clinic, we're committed to providing a minimally invasive procedure for this group."
For more information
Jackson C, et al. Minimally invasive biopsies of deep-seated brain lesions using tubular retractors under exoscopic visualization. Journal of Neurological Surgery Part A: Central European Neurosurgery. 2017;78:588.