Nov. 09, 2019
Mayo Clinic is among a handful of centers in the United States that offer fetoscopic repair of myelomeningocele. The procedure can provide surgical outcomes for the fetus that are similar to those of open surgery while lessening the risk of preterm birth.
"There's a big learning curve for this minimally invasive surgery, which we have met through extensive training and simulations. We believe that the challenge is worthwhile to achieve more full-term deliveries of these babies," says Edward S. Ahn, M.D., a neurosurgeon at Mayo Clinic in Rochester, Minnesota.
Open surgery has been the standard of care for prenatal myelomeningocele repair. Although the open procedure generally improves outcomes for children with myelomeningocele, it increases the risks of preterm birth and uterine rupture. Women who have open surgery for prenatal myelomeningocele repair must have a cesarean section for that pregnancy and all future pregnancies, as well as wait at least two years before becoming pregnant again.
"The objective of fetoscopic repair is to achieve the same outcomes for the babies but reduce maternal obstetric risks," says Rodrigo Ruano, M.D., Ph.D., chair of Maternal and Fetal Medicine at Mayo Clinic's campus in Minnesota. "After fetoscopic surgery these women will be able to have vaginal delivery during that pregnancy and any future pregnancies."
Large, multidisciplinary team
Fetoscopic myelomeningocele repair requires an integrated team of specialists. At Mayo Clinic, that team includes neurosurgeons with experience in intrauterine procedures, maternal and fetal medicine surgeons, pediatric and adult anesthesiologists, pediatric cardiologists to continuously monitor fetal cardiography, and specialized nursing support. "We could not accomplish a successful intervention without this strong collaboration," Dr. Ruano says.
Myelomeningocele is generally diagnosed through routine fetal ultrasound during the second trimester of pregnancy. The surgery can be performed between 19 and 26 weeks of gestation. "We usually prefer to do the procedure at around 24 or 25 weeks, when the fetus is a little bit bigger," Dr. Ahn says.
Fetoscopic repair of a myelomeningocele
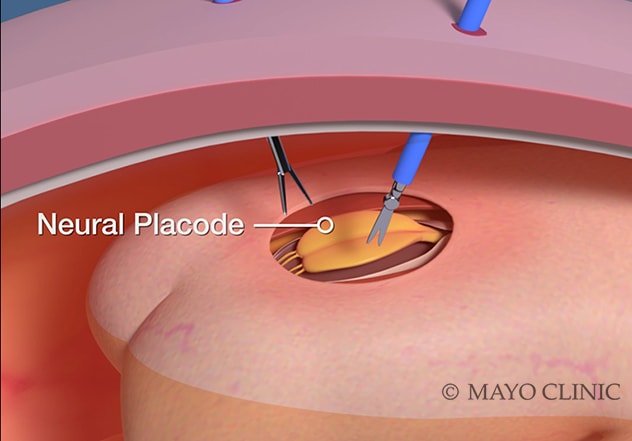
Fetoscopic repair of a myelomeningocele
The fetoscopic repair is performed by inserting 2-millimeter instruments through tiny ports.
The fetoscopic procedure takes about 2.5 hours. General anesthetic is first given to the mother. That anesthetic relaxes the uterus and the fetus before the fetus receives intramuscular pain medication. Carbon dioxide is inserted into the uterus to improve visualization of the spinal defect. The repair is performed by inserting 2-millimeter instruments through tiny ports.
Babies who have prenatal myelomeningocele repair generally experience fewer complications than do babies who have postnatal treatment. Prenatal repair reduces the incidence of Chiari malformation, which can occur when cerebrospinal fluid leaks through the myelomeningocele. "The Chiari malformation will not reverse without intervention," Dr. Ruano says. "But we have an 80% to 90% chance of reversal if the myelomeningocele is fixed in utero."
Chiari malformation can lead to hydrocephalus. "The increase in prenatal myelomeningocele repair has dramatically reduced the incidence of hydrocephalus in these babies," Dr. Ahn says. "Only about 40% of babies with myelomeningocele require treatment for hydrocephalus, compared with 80% previously."
Prenatal repair also prevents the spinal cord's exposure to amniotic fluid, which may be toxic to the spinal cord. "In the long term, babies whose myelomeningoceles are closed prenatally tend to have better leg function," Dr. Ahn says.
Mayo Clinic's obstetric and pediatric specialists have experience caring for babies born with myelomeningocele. The Cerebral Palsy/Spina Bifida Clinic on the Minnesota campus coordinates care for children and teenagers with spina bifida.
"Mayo Clinic is structured to provide multidisciplinary care," Dr. Ahn says. "From simple matters such as scheduling appointments to the routine conferring of specialists, everything is well coordinated."