March 26, 2022
Axial T2-weighted MRI scan with contrast
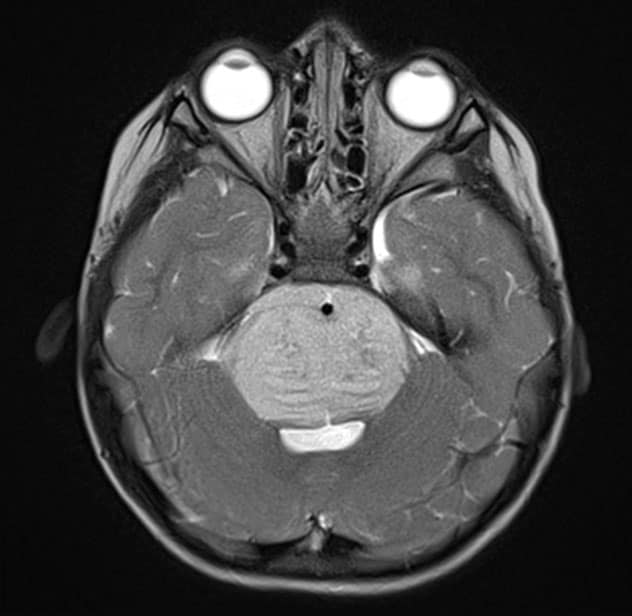
Axial T2-weighted MRI scan with contrast
Axial T2-weighted MRI scan with contrast demonstrates the typical appearance of a newly diagnosed diffuse midline glioma. The patient presented with new-onset ataxia and underwent a biopsy, which confirmed the presence of an H3KM-mutated glioma. The patient received fractionated radiation therapy.
Sagittal T1-weighted MRI scan with contrast
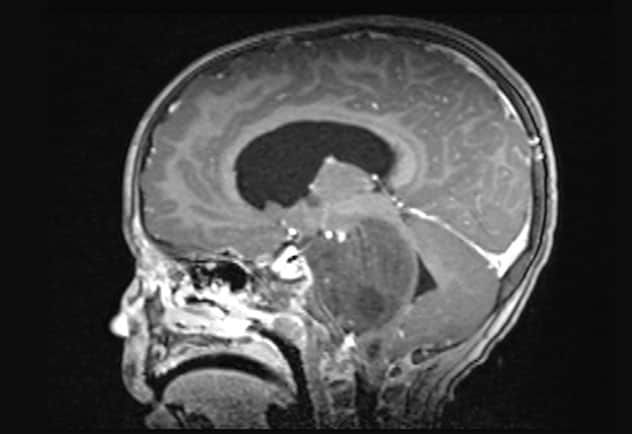
Sagittal T1-weighted MRI scan with contrast
Sagittal T1-weighted MRI scan with contrast demonstrates the typical appearance of a newly diagnosed diffuse midline glioma. The patient presented with new-onset ataxia and underwent a biopsy, which confirmed the presence of an H3KM-mutated glioma. The patient received fractionated radiation therapy.
Mayo Clinic is committed to improving the treatment of diffuse midline glioma, a rare tumor that typically occurs in young children and is fatal within a year. The only beneficial treatment to date has been radiation therapy, which slows disease progression and marginally improves survival.
Mayo Clinic is investigating two new approaches: fractionated radiation therapy and convection-enhanced delivery of anti-cancer medication.
"Diffuse midline glioma is an earth-shattering diagnosis for the family and the child," says Anita Mahajan, M.D., a radiation oncologist at Mayo Clinic Children's Center in Rochester, Minnesota. "None of the 100-plus medications that have gone through clinical trials have ever shown benefits," says David J. Daniels, M.D., Ph.D., a pediatric neurosurgeon at Mayo Clinic Children's Center and director of the Experimental Drug and Therapeutics for Pediatric Brain Tumor Laboratory. "The bottom line is, we need something that works."
Split-course radiation
Standard-of-care treatment for diffuse midline glioma is six weeks of radiation therapy. A second six-week course has been attempted when symptoms arise. "But treating the same area twice with high doses of radiation comes at a cost in terms of brain toxicities," Dr. Mahajan says.
To lessen those effects, Mayo Clinic's new protocol splits the standard-of-care six-week radiation course. Children have an initial two weeks of radiotherapy followed by close monitoring. "We delay the second two-week course until there is some evidence that the tumor is acting up. If need be, we give a third two-week round later," Dr. Mahajan says. "We still monitor and treat the tumor. But this is an opportunity to use radiation more strategically."
Mayo Clinic is assessing the time intervals between patients' first and second radiation courses, as well as any effects on treatment and survival from splitting the radiation course. Children and their families also are asked to complete questionnaires measuring quality of life.
Improving quality of life is the new protocol's primary goal. "Spending time at home participating in normal daily activities, instead of days in the hospital, is what makes a child's and family's quality of life better," Dr. Mahajan says. Controlling tumors through shorter radiation courses also can allow children to stop taking medications such as steroids that can cause difficult side effects.
"We're going to be with our patients through anything that presents. We want to have a positive impact on their lives," Dr. Mahajan says.
Convection-enhanced delivery
Convection-enhanced delivery is a method of bypassing the blood-brain barrier and transporting medication directly to a tumor. Mayo Clinic is participating in an upcoming multisite study that will use that method to deliver an antibody drug conjugate.
"Diffuse midline gliomas likely have an intact blood-brain barrier," Dr. Daniels says. "The reason why drugs consistently fail is multifactorial. But one big hurdle is that we're just not getting the drugs to the tumors."
Demonstrating a safe and effective method of delivering medication to diffuse midline gliomas could facilitate future studies of new therapies. Mayo Clinic's laboratory investigating experimental drugs for pediatric brain tumors has cured some rodent models of the disease.
Mayo Clinic's research efforts bring together a multidisciplinary team of neuroradiologists, neurosurgeons, oncologists and pathologists. "We are all on board with advancing the science," Dr. Mahajan says. "We are learning so much and hope to continue to improve the way we approach this disease."
For more information
Experimental Drug and Therapeutics for Pediatric Brain Tumor Laboratory: David J. Daniels. Mayo Clinic.
Refer a patient to Mayo Clinic.