Feb. 28, 2020
Alfonso (Sebastian) S. Lopez Chiriboga, M.D., and Iris (Vanessa) V. Marin Collazo, M.D., neurologists in Multiple Sclerosis and Autoimmune Neurology at Mayo Clinic in Jacksonville, Florida, discuss autoimmune neurology, one of neurology's most rapidly evolving subspecialties.
What is autoimmune neurology?
Autoimmune neurology encompasses immune-inflammatory diseases of the central nervous system (CNS) other than multiple sclerosis (MS). The autoimmune neurology subspecialty is driven by recent discoveries of multiple autoantibodies that target proteins expressed in the CNS. Those discoveries helped to increase recognition of autoimmunity as the cause of neurological conditions misdiagnosed as primarily psychiatric disorders, degenerative diseases such as dementia or infections.
Autoimmune neurology interacts with many other subspecialties, including behavioral neurology, epilepsy and movement disorders, as well as other medical specialties, including rheumatology, gastroenterology, oncology and psychiatry.
What types of conditions are seen in patients at Mayo's MS/autoimmune clinic?
Most patients have antibody-mediated CNS disorders such as autoimmune encephalitis or autoimmune epilepsy, or an autoimmune movement disorder such as stiff person syndrome or ataxia. The clinic team also evaluates and provides care to patients with neuromyelitis optica spectrum disorder (NMOSD), optic neuritis, transverse myelitis and neurosarcoidosis, in addition to MS. The multidisciplinary clinic offers integrated care in a one-time visit.
When should a physician refer a patient to the MS/autoimmune clinic?
Patients who would benefit from referral include those with suspected or confirmed autoimmune encephalitis, NMOSD, optic neuritis, transverse myelitis or neurosarcoidosis. In addition, physicians should consider referral for patients with:
- Neurological symptoms in the setting of a diagnosis of cancer
- New-onset epilepsy with no clear explanation, especially if seizures have been refractory to more than one anti-epileptic medication
- A history of autoimmunity — such as lupus, Sjogren's disease, Crohn's disease, rheumatoid arthritis or sarcoidosis — and the development of new neurological symptoms suspicious for CNS involvement
At Mayo Clinic, these patients are seen by autoimmune neurologists. Why is that distinction important?
The complexity of the clinical presentations, the longitudinal follow-up and the medications used for these disorders require expertise in the optimal management of these conditions. Mayo Clinic's autoimmune neurologists have formal fellowship training in their subspecialty.
Many disorders can be mistaken as autoimmune encephalitis. Use of unnecessary immunotherapy in patients can have serious adverse effects, including the potential risk of severe infections or cancer. Mayo Clinic noted, in research published in Neurology in 2017, the importance of being evaluated by an autoimmune neurologist subspecialist to avoid these problems.
Additional research indicates that autoimmune encephalitis is more common than previously known. In the Annals of Neurology in 2018, Mayo Clinic published results of the first population-based comparison study of autoimmune encephalitis and infectious encephalitis. Our study found that the prevalence and incidence of autoimmune encephalitis are comparable to infectious encephalitis, and the detection of autoimmune encephalitis is increasing over time.
What is Mayo Clinic's approach to the diagnosis and treatment of autoimmune neurological conditions?
Patients are seen by physicians with expertise in diagnosing and managing the sequelae of CNS autoimmunity — not only neurologists but also psychiatrists, rheumatologists and neuropsychologists. In addition, patients are in close contact with nursing staff with expertise in managing symptoms and monitoring immunotherapy. Under Mayo Clinic's multidisciplinary approach, patients may also be seen by specialists in epilepsy, behavioral neurology or movement disorders, to ensure the best possible care and recommendations.
MRI and PET images of patient with autoimmune encephalitis
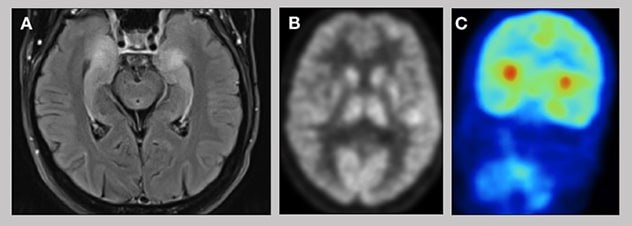
MRI and PET images of patient with autoimmune encephalitis
A. MRI of a patient with autoimmune encephalitis shows inflammatory changes in the temporal lobes bilaterally. B and C. Brain 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET) of a patient with autoimmune encephalitis shows areas of hypermetabolism in the basal ganglia and temporal lobes.
Autoimmune neurological disorders require expert evaluation to provide an accurate diagnosis. Mayo Clinic's state-of-the-art resources include high-field MRI and a dedicated immunology laboratory for the diagnosis, treatment, rehabilitation and longitudinal care of patients with these disorders. Test results and treatment plans are typically generated in less than two weeks.
There are no FDA-approved medications for most autoimmune neurological diseases. But Mayo Clinic is at the forefront of studying new therapies and treatment protocols. Patients benefit from the most current therapeutic options.
For more information
Lopez-Chiriboga AS, et al. Emerging subspecialties in neurology: Autoimmune neurology. Neurology. 2017;89:e129.
Dubey D, et al. Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Annals of Neurology. 2018;83:166.