Dec. 23, 2015
Encephalopathies — typically characterized by confusion, seizures, memory loss and behavioral changes — have been well-recognized as having an autoimmune cause. In contrast, patients with progressive dementia without delirium have usually been classified as having neurodegenerative disease.
Building on the pioneering work of Vanda A. Lennon, M.D., Ph.D., a consultant in the Mayo Clinic Neuroimmunology Research Laboratory, neurologists at Mayo Clinic in Rochester, Minnesota, have found that patients whose symptoms mimic those of neurodegenerative dementias can actually have an autoimmune cause for their conditions. Although autoimmune dementia responds to immunotherapy, the disease often goes untreated because of misdiagnosis as a neurodegenerative or psychiatric condition.
"It can be devastating for patients to be labeled with a neurodegenerative disease but actually have an immune-mediated dementia, because they're missing out on a treatment that can reverse their symptoms," says Eoin P. Flanagan, M.B., B.Ch., a consultant in Neurology at Mayo Clinic in Rochester, Minnesota. "If treatment is delayed, patients tend not to respond as well. It's important to recognize this condition because you might miss your opportunity for treatment."
A nose for atypical disease
Among patients at Mayo Clinic who responded to immunotherapy for autoimmune dementia from 2002 to 2009, 35 percent were initially misdiagnosed with a neurodegenerative disorder. Mayo Clinic neurologists have also used immunotherapy to successfully treat patients who experienced a rapidly progressing dementia and were initially diagnosed with Creutzfeldt-Jakob disease.
Patients with autoimmune dementia typically present with some, but certainly not all, clinical and laboratory features associated with limbic encephalitis. Clinical and laboratory features of autoimmune dementia include:
- Subacute onset
- Fluctuating course
- Tremor
- Headache
- Personal or family (first-degree relative) history of autoimmunity
- History of recent or past neoplasia
- Evidence of central nervous system inflammation from cerebral spinal fluid or MRI
- Detection of neural antibody
Abnormalities in temporal lobe and basal ganglia
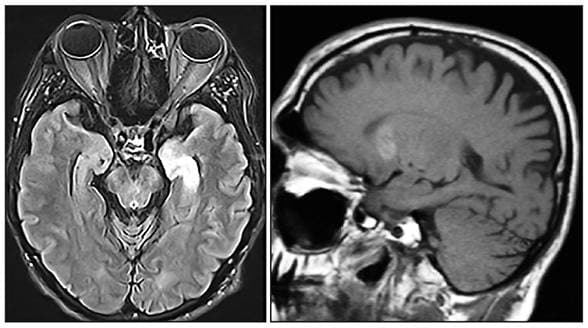
Abnormalities in temporal lobe and basal ganglia
On the left, MRI shows abnormal T2 hyperintensity in the left mesial temporal lobe in a patient with autoimmune dementia due to antibodies to the leucine-rich, glioma-inactivated 1 (LGI1) protein, a component of the voltage-gated potassium channel complex. On the right, MRI shows abnormal T1 hyperintensity within the basal ganglia in a patient with autoimmune dementia and accompanying faciobrachial dystonic seizures due to LGI1 autoantibodies.
PET scan showing prominent hypometabolism
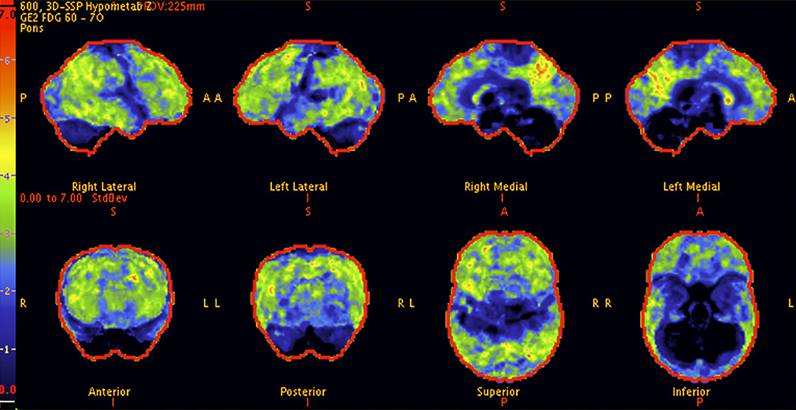
PET scan showing prominent hypometabolism
PET scan of a 68-year-old woman with a history of lupus and a 10-year history of cognitive difficulties. The scan shows prominent hypometabolism with a pattern suggestive of Alzheimer's disease.
PET scan after treatment with immunosuppressants
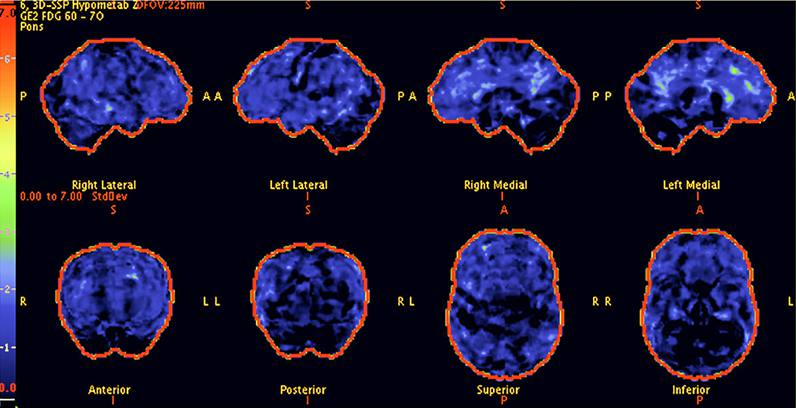
PET scan after treatment with immunosuppressants
PET scan of the patient after treatment with immunosuppressants. Normalization of the scan was associated with dramatic improvement in cognitive abilities.
MRI might show abnormalities in the limbic lobes or elsewhere; PET imaging might show hypometabolism. Cognitive decline, particularly memory loss, is the predominant symptom. But patients can also have hallucinations and a fluctuating course of disease.
"It's important to look for atypical disease," says Daniel A. Drubach, M.D., a consultant in Neurology at Mayo Clinic's campus in Minnesota. "For example, when a patient is diagnosed at 45 years of age with schizophrenia, that raises a red flag. I have seen many patients with an autoimmune-based dementia who were in psychiatric hospitals."
"It comes down to the clinician having a good nose for this diagnosis," adds Sean J. Pittock, M.D., a consultant in Neurology and director of the Center for Multiple Sclerosis and Autoimmune Neurology at Mayo Clinic's campus in Minnesota. "You look for the clues that tell you this isn't just run-of-the-mill neurodegenerative disease."
Mayo Clinic has developed a standardized approach to diagnostic evaluation of suspected autoimmune neurological disorders, based on three M's:
- Maximum reversibility — also called the "diagnostic test" — determined by comparison of objective baseline testing of main deficits compared with post-immunotherapy testing
- Maintenance of reversibility, using long-term immunotherapy in chronic autoimmune diseases
- Minimal therapeutic dosage to reduce the side effect profile
To assist with diagnosis, Mayo Clinic is the first center in the U.S. to offer biomarker testing for autoimmune dementia. Serum and cerebral spinal fluid are evaluated for neural antibodies associated with the condition. Consultative comments from Mayo Clinic neurologists accompany test findings.
"The panel results must be interpreted in the clinical context because there are patients with Alzheimer's disease who have low titers of some of these antibodies," Dr. Pittock says. Mayo Clinic consultants are also available to discuss test results over the telephone with referring neurologists.
Autoimmune dementia evaluation
A comprehensive autoimmune dementia evaluation for serum and cerebral spinal fluid is available from Mayo Medical Laboratories. The evaluation provides neurologists with neural antibody testing for patients with symptoms of autoimmune dementia. Mayo Clinic neurologists provide interpretation of test results and are available for consultation with referring physicians. Testing must be ordered by a hospital laboratory.
Treatment and response
Acute treatment for autoimmune dementia generally involves intravenous steroids once a day for five days. "If patients improve, and do indeed have an autoimmune dementia, it usually occurs within the first week of treatment. A smaller minority will start to improve within the first month," Dr. Flanagan says. For more-sustained improvement, patients sometimes have immunotherapy once a week for six to 12 weeks.
To measure cognitive change, patients are given the Kokmen Short Test of Mental Status or more-detailed neuropsychological testing at the beginning and end of treatment. MRI and spinal fluid testing are also often done before and after treatment. "Patients may not go back to normal," Dr. Drubach says. "But they may do better than those without treatment."
At Mayo Clinic, patients benefit from the close interaction between physician-researchers with expertise in autoimmunity and behavioral neurology. Dr. Flanagan has training in both. "It's generally thought that dementias are always neurodegenerative," he says. "But we're at only the tip of the iceberg in terms of discovering neural antibodies. It's important to look out for these atypical dementia cases because they can respond very well to immunotherapy."