Sept. 21, 2022
Mayo Clinic is one of the few centers that routinely uses 7-Tesla (7-T) MRI to assess individuals with epilepsy. That advanced imaging technology can better detect epileptogenic lesions, such as focal cortical dysplasia, compared with conventional 3-Tesla (3-T) MRI.
"Approximately 40% of patients whose 3-T MRI results are normal will have a presumably causative lesion identified with 7-T MRI. We can see very small and difficult-to-visualize anatomy in extreme detail — things we never saw with standard field strength," says Erik H. Middlebrooks, M.D., a neuroradiologist at Mayo Clinic in Jacksonville, Florida.
7-T MRI provides a magnetic field more than twice as strong as that of conventional 3-T MRI. That extra field strength greatly enhances the signal-to-noise ratio, thereby improving clarity, contrast and resolution.
"Our chances of providing seizure freedom go up significantly if we can identify a lesion on preoperative imaging," says Sanjeet S. Grewal, M.D., a neurosurgeon at Mayo Clinic's campus in Florida. "We see patients who have had epilepsy for decades and been told there's no visible lesion. But on 7-T MRI, it's almost as clear as day."
As a major tertiary center, Mayo Clinic can meet the challenges of implementing 7-T MRI. "It's not as simple as just doing 3-T sequences at higher resolution. The 7-T platform requires a lot of sequence development and redesign," Dr. Middlebrooks says. "Our experienced team of physicians and physicists have been a driving force to help us apply 7-T strength to clinical imaging."
Multidisciplinary search for answers
Enhanced visualization
Enhanced visualization
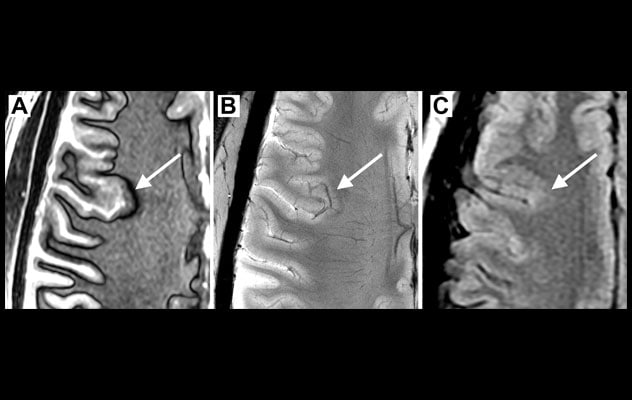
A. MRI using a novel sequence developed at Mayo Clinic — known as 3D-EDGE — and adapted to 7-Tesla (7-T) MRI clearly shows a focal cortical dysplasia (arrow). B. 7-T ultrahigh resolution T2* image at 200-micron resolution reveals disruption of normal cortical lamination and grey matter-white matter boundary (arrow). C. Multiple 3-T MRI scans failed to show the lesion in the same area, (arrow) as shown on 3-T fluid-attenuated inversion recovery scans.
Mayo Clinic in Rochester, Minnesota, was the first center in North America to use clinical 7-T MRI after the system was approved. Enhanced visualization is a key part of Mayo Clinic's multidisciplinary approach to medication-refractory epilepsy enterprisewide.
Neurologists, neuroradiologists and neurosurgeons meet regularly to assess 7-T MRI findings alongside a patient's electroencephalography (EEG) testing. CT and single-photon emission computed tomography (SPECT) scans also are sometimes performed. If multiple lesions are identified, intracranial stereo-EEG can determine precisely which lesions are contributing to an individual's seizures.
"We integrate our imaging data, patient's seizure semiology and electrophysiologic data to devise a treatment strategy," Dr. Grewal says.
The options include laser ablation and neuromodulation, including vagus nerve stimulation, direct brain stimulation and responsive neurostimulation. If resection is recommended, awake surgery might be an option.
"Our multidisciplinary team performs these awake procedures with the goal of removing as much of the seizure onset zone as possible without causing neurological deficits," Dr. Grewal says.
7-T MRI particularly excels at locating lesions associated with focal cortical dysplasia. Drs. Middlebrooks and Grewal recently treated a young adult who had experienced medication-refractory seizures since adolescence. The patient came to Mayo Clinic when imaging at another center couldn't locate a seizure origin site. That center had recommended intracranial surgery to identify the site.
At Mayo Clinic, the patient had 7-T MRI instead.
"The subtle lesions associated with focal cortical dysplasia are notoriously difficult to find on MRI," Dr. Middlebrooks says. "But with 7-T MRI, we found a dysplasia that correlated perfectly with the patient's seizure workup."
Dr. Grewal performed laser ablation. "The patient was able to go home the next day and has been seizure-free ever since," Dr. Grewal says. "It's been life-altering for him."
For more information
Refer a patient to Mayo Clinic.