Sept. 14, 2018
A 41-year-old man with multiple endocrine neoplasia, type 1 (MEN1) presented for management of recurrent primary hyperparathyroidism (PHPT). He had undergone a 3.5 parathyroid gland resection at age 22. At age 33, 11 years after his initial subtotal parathyroidectomy, his serum calcium concentration was noted to be mildly elevated at 10.2 mg/dL (normal, 8.9 to 10.1 mg/dL) and was associated with an elevated parathyroid hormone (PTH) level and normal serum creatinine. No further interventions were recommended because he was asymptomatic.
At age 39, he continued to be in good health, but his serum calcium level was 10.9 mg/dL on two separate occasions, in the setting of elevated serum PTH levels and normal serum creatinine — findings consistent with recurrent PHPT. A parathyroid sestamibi scan showed uptake consistent with a right inferior parathyroid adenoma. Treatment options were discussed with the patient by a multidisciplinary team involving his endocrinologist, endocrine surgeon and interventional radiologist. The team made a final recommendation to pursue percutaneous ethanol ablation (PEA).
Right inferior parathyroid adenoma
Right inferior parathyroid adenoma
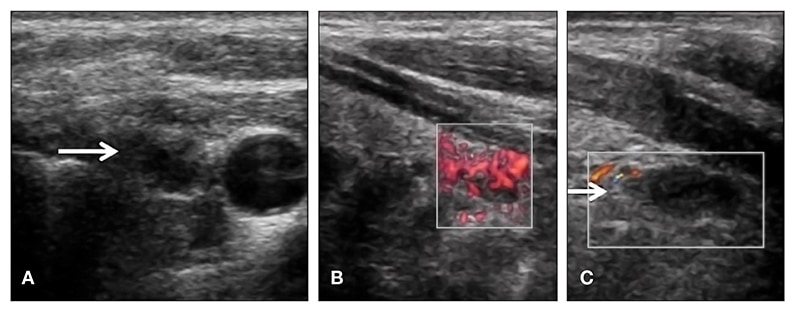
Panels A and B. Right inferior parathyroid adenoma on axial ultrasound image (A) and sagittal ultrasound image (B) measuring 9 mm and with detectable blood flow before ethanol injection. Panel C. Right inferior parathyroid adenoma on sagittal ultrasound image is approximately the same size but with undetectable blood flow after ethanol injection.
A neck ultrasound was performed to identify a potential target for PEA and showed a 9 mm right inferior parathyroid adenoma. The ultrasound was consistent with the finding on the parathyroid sestamibi scan. The patient was treated with a percutaneous 0.3 mL ethanol injection. The calcium level the day after the procedure was 9.6 mg/dL, and the vascularity of the parathyroid tissue resolved.
However, recurrent hypercalcemia two years later prompted a second injection of ethanol — the patient required two sessions of PEA (total volume of 0.6 mL) into a 7 mm adenoma seen on neck ultrasound. He tolerated both procedures without complications such as hypocalcemia, hoarseness, bleeding or infection. Follow-up three years later shows that he continues to have normal serum calcium levels and is in overall good health.
MEN1 is a rare endocrine disorder characterized by loss of function of the tumor suppression protein MENIN, leading to the development of tumors in endocrine glands. Most commonly the parathyroid glands are affected, leading to PHPT. The clinical presentation of patients with PHPT and MEN1 differs from those with sporadic PHPT; patients with MEN1 have an earlier onset and commonly more-severe disease. Most importantly, the rate of recurrence after initial surgery in these patients is higher (up to 67 percent).
At this time, there is no clear consensus about which of the available treatment options provides the most benefit to these patients while limiting risk. Treatment options include re-operation, PEA and medical treatment with cinacalcet. Surgical intervention is able to resolve hypercalcemia in the majority of patients but carries a significant risk of hypoparathyroidism (approximately 10 percent), which can affect the quality of life of these patients. PEA, although not available in many centers, is considered an effective and overall safe treatment option.
The main difference between these two treatment approaches is the need for repeated injection in patients who receive PEA (mean duration of eucalcemia is approximately 24 months), since this treatment appears to control the disease but does not provide a definitive cure. On the other hand, re-operation might be considered a more definitive approach but has a higher risk of hypoparathyroidism.
Moreover, when to re-intervene in these patients is also a matter of debate, given the limitations of the available treatment options. Observation in cases of recurrence associated with mild hypercalcemia in patients who are asymptomatic might be a reasonable option.
Key message
PHPT is the most common clinical manifestation of patients with MEN1 and is associated with high recurrence rates after initial surgical intervention. A discussion of the risks and benefits of each of the available treatment options should be carried out by an experienced multidisciplinary team in the setting of the patient's values and preferences to provide the patient with the treatment recommendation that best fits his or her needs.