Sept. 15, 2018
With the increased use of high-resolution neck ultrasonography, thyroid nodules are commonly detected in clinical practice. When a thyroid nodule is cystic, the American Thyroid Association advises that pure cysts are of negligible malignancy risk (less than 1 percent) and partially cystic nodules with no suspicious features are considered very low suspicion (less than 3 percent risk of malignancy). Once malignancy has been excluded, treatment paths are dictated by the presence or absence of symptoms, such as compressive symptoms.
Marius N. Stan, M.D., with Endocrinology, Diabetes, Metabolism, and Nutrition at Mayo Clinic's campus in Rochester, Minnesota, says: "Treatment options for symptomatic benign cystic or predominately cystic thyroid nodules include needle aspiration, minimally invasive techniques or surgical resection. With needle aspiration the recurrence rates are high (60 to 90 percent). Although surgical management is definitive, it can be associated with complications — leading some patients to decline this treatment option. In addition, in some patients (because of medical comorbidities) surgery is contraindicated.
"In these clinical scenarios, a minimally invasive treatment option, such as percutaneous ethanol injection (PEI) under ultrasound guidance, generally should be considered. With thyroid cyst PEI, the ethanol results in permanent tissue damage with subsequent necrosis, fibrosis and thrombosis of cyst wall blood vessels."
M. Regina Castro, M.D., with Endocrinology, Diabetes, Metabolism, and Nutrition at Mayo Clinic's campus in Minnesota, says: "We recently published a study in Mayo Clinic Proceedings where we determined the safety and efficacy of PEI in the treatment of cystic thyroid nodules."
Nicole M. Iñiguez-Ariza, M.D., a research fellow with Endocrinology, Diabetes, Metabolism, and Nutrition at Mayo Clinic's campus in Minnesota, explains: "In the study, safety was defined as either no adverse events or minor adverse events such as temporary pain. Efficacy was defined as symptom relief, reduction in nodule volume by 50 percent or more, or both. Twenty patients with cystic thyroid nodules were treated with PEI; eight patients had pure thyroid cysts and 12 patients had complex cystic thyroid nodules — nodules that had more than 50 percent cystic component."
Robert A. Lee, M.D., with Radiology at Mayo Clinic's campus in Minnesota, notes: "The largest median diameter of the thyroid cyst was 4.5 cm (range, 2.3 to 8.0 cm); the median volume before PEI was 19.6 mL (range, 2.8 to 118.1 mL). The median amount of cystic fluid drained prior to PEI was 13.5 mL, and the median amount of ethanol administered was 3 mL (range, 0.5 to 20 mL).
Thyroid cyst before and at follow-up after PEI
Thyroid cyst before and at follow-up after PEI
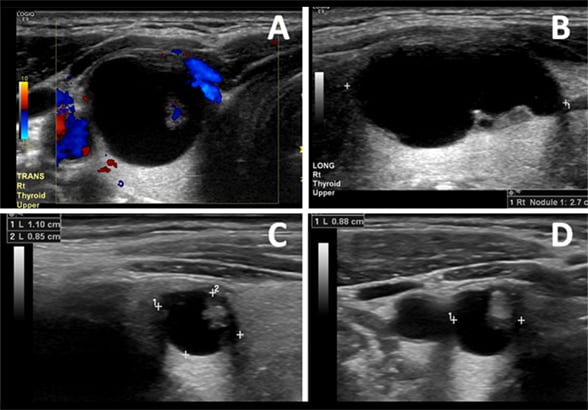
Example of a thyroid cyst before and at follow-up after percutaneous ethanol injection (PEI). Panels A and B, transverse and longitudinal views of cystic nodule before PEI; 1.4 by 1.4 by 2.7 cm and volume of 2.77 cc. Panels C and D, transverse and longitudinal views of the cystic nodule 12 months after PEI; 1.1 by 0.85 by 0.88 cm and volume of 0.43 cc (84 percent volume reduction).
"At follow-up (median follow-up was two years), 89 percent of patients were asymptomatic, and 70 percent had a 50 percent or greater reduction in nodule volume. The median decrease in volume was 75.6 percent. Four patients (20 percent) had mild and temporary side effects such as vagal reaction, slight pain and bleeding into the cyst."
Dr. Castro concludes: "Our study demonstrates that PEI is a safe and effective treatment option in patients with large, benign, symptomatic cystic nodules. In the era of minimally invasive treatments and shared decision-making, the availability of PEI for treatment of otherwise benign thyroid disease is an attractive treatment option. Our findings can be used to counsel patients interested in alternative treatment options to surgery."
For more information
Iñiguez-Ariza NM, et al. Ethanol ablation for the treatment of cystic and predominantly cystic thyroid nodules. Mayo Clinic Proceedings. 2018;93:1009.