June 09, 2018
A 42-year-old man was referred to Mayo Clinic by his local physician for further evaluation of a flushing disorder. His symptoms began about seven years previously. At that time he would flush only if he had an alcoholic beverage and occasionally after a large meal or exercise.
About four years before coming to Mayo Clinic, he started flushing without obvious triggers and his symptoms worsened — by the time of presentation, he had three to four facial flushing episodes each day lasting 15 to 20 minutes and primarily involving his face and neck. With these episodes, he did not have any shortness of breath, diarrhea or sweating. He did not have hypertension.
Over the past four years, he had developed a persistent red rash over his back, chest and upper arms, which was reported unremarkable on skin biopsy performed two years previously. Over the past couple of years, he had also developed a sense of temperature dysregulation. He was not taking any regular medication, and there was no clinically significant family or social history.
Patient before and after surgery
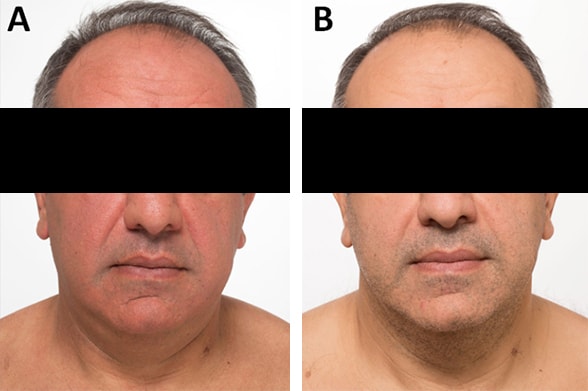
Patient before and after surgery
Photographs taken before (A) and three months after (B) surgery to resect medullary thyroid cancer.
On physical examination, he had a moderately flushed face and a diffuse red rash over his back. With his arms raised his facial flush did not change. The thyroid appeared normal on examination, without any nodules appreciated on palpation. The remainder of the physical examination was normal. Normal laboratory studies included:
- Complete blood count and routine chemistries
- Serum serotonin; serum tryptase
- 24-hour urine for 5-hydroxyindoleacetic acid, N-methylhistamine, fractionated metanephrines and catecholamines
The 24-hour urine for 2,3-dinor-11beta-prostaglandin F2-alpha was mildly increased at 1,363 ng (normal, < 1,000 ng). Skin biopsies showed multiple telangiectasias and no sign of mast cell abnormalities.
Tests for other potential causes of flushing disorder were obtained, which were remarkable for a serum calcitonin concentration markedly elevated at 552 pg/mL (normal < 16 pg/mL). Based on this information, thyroid ultrasound was obtained.
Ultrasound of the thyroid showed a 1.8-cm suspicious nodule in the midright thyroid lobe. Fine-needle aspiration biopsy findings were consistent with medullary thyroid carcinoma (MTC). Bidirectional sequence analysis was performed to test for the presence of a mutation in exons 10, 11, 13, 14, 15 and 16 of the RET proto-oncogene and was negative.
He underwent a near-total thyroidectomy, and pathology showed that the MTC formed a 1.8-by-1.4-by-1.1-cm mass. He also had an incidental 0.7-cm papillary thyroid carcinoma in the midportion of the right lobe of the thyroid. After surgery, he had complete resolution of his symptoms of flushing and the rash. At his six-month follow-up visit, he had an undetectable serum calcitonin concentration and a normal serum concentration of carcinoembryonic antigen. Neck ultrasound showed no evidence of adenopathy.
Discussion
Ultrasound of a 1.8-cm nodule in right thyroid lobe
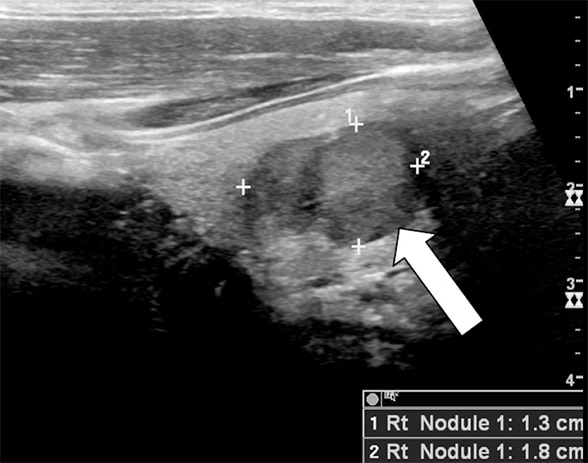
Ultrasound of a 1.8-cm nodule in right thyroid lobe
Thyroid ultrasound image showing a 1.8-cm nodule in right thyroid lobe (arrow), which proved to be medullary thyroid cancer.
As highlighted in a review published in the Journal of the American Academy of Dermatology in 2006, flushing is a sensation of warmth accompanied by transient erythema that most commonly occurs on the face, but may also involve the neck, ears, chest, epigastrium, and arms or other areas. The most common etiologies for which a patient will present with flushing are fever, hyperthermia, primary gonadal failure such as menopause, emotional blushing and rosacea.
When an etiology is not identified by history and physical examination, initial laboratory evaluation includes:
- A complete blood count and liver function tests
- 24-hour urine for 5-hydroxyindoleacetic acid to screen for carcinoid syndrome
- Serum tryptase and 24-hour urine for methylhistamine, 2,3-dinor-11beta-prostaglandin F2-alpha, and leukotriene E4 to screen for mast cell disease
- Markers for other potential etiologies such as serum calcitonin
In this case, an elevated calcitonin led to further investigations, diagnosis and cure. Blood concentrations of calcitonin are elevated in patients with medullary thyroid cancer. In patients with thyroid nodules, however, the routine assessment of serum calcitonin is controversial, and the American Thyroid Association guidelines published in Thyroid in 2016 do not recommend for or against routine measurement of serum calcitonin in patients with thyroid nodules.
False-positive calcitonin results may be obtained in patients with hypercalcemia, hypergastrinemia, neuroendocrine tumors, renal insufficiency, papillary and follicular thyroid carcinomas, goiter, chronic autoimmune thyroiditis, and prolonged use of certain medications. A false-negative test result may be seen in rare medullary thyroid cancers that do not secrete calcitonin.
For more information
Izikson L, et al. The flushing patient: Differential diagnosis, workup, and treatment. Journal of the American Academy of Dermatology. 2006;55:193.
Haugen BR, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1.