April 18, 2020
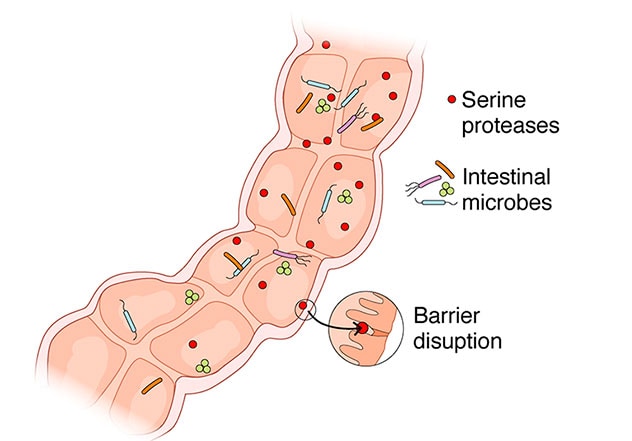
Serine and cysteine proteases are the most abundant family of fecal proteases. Prior research has established that ileostomy contents have significantly higher and qualitatively different proteolytic activity (PA) than feces. And germ-free or microbiota-depleted mice following administration of antibiotics have higher levels of fecal PA than normal mice. Thus, many experts now hypothesize that microbiota present in the colon play important roles in modulating PA, and that PA becomes depleted during colonic transit, either due to the direct effects of microbiota or from the effects of microbiota on the host.
Elevated PA levels have been observed in fecal and tissue supernatants from patients with diarrhea and constipation-predominant irritable bowel syndrome (IBS-C). Researchers studying these conditions have also noted increased intestinal permeability and visceral hypersensitivity when these supernatants are administered in mice.
Building on this knowledge, Mayo Clinic researchers recently conducted a study to determine the effects of proteases on intestinal barrier function in individuals with post-infection IBS (PI-IBS) and IBS-C, and to associate it with clinical symptoms and microbiota composition. The results of their study were published in Gut in 2020.
Study methods
The study enrolled 39 patients with IBS and 25 healthy volunteers who completed questionnaires and underwent additional assessments. The researchers performed assessments of in vivo permeability, ex vivo colonic barrier function in Ussing chambers, tight junction proteins, and ultrastructural morphology, 16S gene sequencing of fecal microbiota rRNA, and a casein-based assay to measure PA in fecal supernatants. And they evaluated PA and intestinal barrier function in germ-free mice after administering human feces with high or low levels of PA.
Significant findings
Intestinal proteases under the control of commensal gut microbiota affect barrier function of the intestinal epithelium
Intestinal proteases under the control of commensal gut microbiota affect barrier function of the intestinal epithelium
Patients with high proteolytic activity in feces have worse IBS symptoms and a disrupted colonic barrier. Microbes from these patients can transfer this phenotype in germ-free mice, suggesting a direct role of microbiota in affecting the proteases in the gut.
- Fecal PA levels were higher in patients with IBS compared with healthy volunteers. Elevated fecal PA levels were observed in 40% of patients (8/20) with PI-IBS and 16 % (3/19) of patients with IBS-C.
- Patients with elevated fecal PA levels had more frequent and looser bowel movements more-severe symptoms and increased colonic permeability both in vivo and ex vivo.
- Patients with IBS and high PA levels had lower occludin expression, wider tight junctions on biopsies and reduced microbial diversity compared with patients with low PA levels.
- Elevated PA levels in fecal supernatants were associated with disruptions in intestinal barrier permeability via decreased occludin and increased phosphorylated myosin light chain (pMLC) expression.
- Serine protease inhibitors, but not cysteine protease inhibitors, significantly blocked the effects of high-PA fecal supernatants on intestinal barrier function. And pharmacological or siRNA inhibition of protease-activated receptor-2 diminished these effects.
- Germ-free mice that received feces with microbiota from high PA IBS patients had greater in vivo intestinal permeability than mice receiving microbiota from low PA IBS patients.
Conclusions and clinical significance
Overall, this study demonstrates that a subset of patients with IBS, especially those with PI-IBS, have substantially elevated levels of fecal PA, greater severity of IBS symptoms, including worse diarrhea, impaired barrier function and reduced microbial diversity.
"In this study population and subsequently in larger cohorts, we continue to find that about 40% of patients with post-infection IBS have elevated fecal proteolytic activity," says Madhusudan (Madhu) Grover, M.B.B.S. Dr. Grover is a gastroenterologist at Mayo Clinic's campus in Rochester, Minnesota, and the corresponding author of the article published in Gut. "These are individuals who were healthy before, got a foodborne gastroenteritis with campylobacter and now have developed chronic IBS symptoms. Clinically, these patients with high protease activity have more-severe IBS symptoms and gut barrier impairment (or 'leaky gut') than those with low protease activity."
Using cultures, Dr. Grover and colleagues confirmed that the gut microbiota can affect luminal PA, which can, in turn, influence intestinal barrier function. "We established that the fecal supernatants from patients with high protease activity caused much greater disruption of barrier function," explains Dr. Grover. "We also observed that the gut microbial communities in these patients are far less diverse, which has been linked to other inflammatory gut disorders."
Dr. Grover notes that these findings suggest that a relatively simple fecal test for protease activity might provide insight into the gut health of patients with IBS. "It is plausible that these patients with high levels of protease activity will be more suitable for microbiota-based therapies, which can replenish the gut flora, instead of antibiotics, which can further deplete it. Identifying the specific microbes involved and how to best replenish the microflora will require further examination, as conventional strategies using probiotics are often not successful."
Additional research is needed to further clarify which microbes in the gut affect the activity of these proteases and what their mechanism of action is. "To learn more about how proteases affect gut physiology in irritable bowel syndrome we are performing detailed phenotyping of these patients to understand the sensory, motor and barrier problems," explains Dr. Grover. "Furthermore, in conjunction with the microbiome program within Mayo Clinic's Center for Individualized Medicine, we are using gnotobiotic mouse models to study the effects of specific microbiota from patients with IBS. We hope these studies will allow us to decipher mechanisms of protease imbalance in IBS and test strategies for restoring it."
For more information
Edogawa S, et al. Serine proteases as luminal mediators of intestinal barrier dysfunction and symptom severity in IBS. Gut. 2020;69:62.