Overview
Truncus arteriosus
Truncus arteriosus
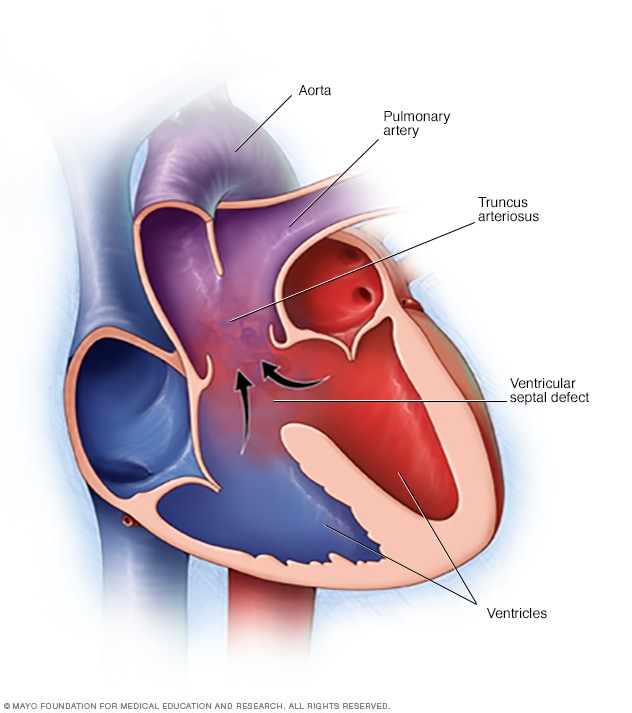
In truncus arteriosus, one large vessel comes out of the heart, instead of two separate ones. There's also usually a hole in the wall between the lower heart chambers, called the ventricles. The hole is called a ventricular septal defect. In truncus arteriosus, oxygen-rich blood, shown in red, and oxygen-poor blood, shown in blue, mix together. The mixed blood is shown in purple. It doesn't contain enough oxygen for the body's needs.
Truncus arteriosus (TRUNG-kus ahr-teer-e-O-sus) is a rare heart condition present at birth. That means it's a congenital heart defect. In this condition, one large blood vessel leads out of the heart, instead of two.
Having only one large blood vessel means that oxygen-poor and oxygen-rich blood mix. This mixing reduces the amount of oxygen delivered to the body. It usually increases the amount of blood flow into the lungs too. The heart has to work harder to adjust for the changes in blood flow.
A baby, also called a fetus, with truncus arteriosus also usually has a hole between the two lower heart chambers, called the ventricles. The hole is called a ventricular septal defect.
Another name for truncus arteriosus is common arterial trunk.
Products & Services
Symptoms
Symptoms of truncus arteriosus most often occur in the first few days of life. They include:
- Blue or gray skin due to low oxygen levels.
- Extreme sleepiness.
- Poor feeding.
- Poor growth.
- Pounding heartbeat.
- Fast breathing.
- Shortness of breath.
When to see a doctor
If you are worried about your baby's feedings, sleep patterns or growth, contact a healthcare professional for an appointment.
Always seek emergency medical care if a baby has any of the following:
- Blue or gray skin.
- Fast breathing.
- Shallow breathing.
- Any breathing trouble.
Causes
Truncus arteriosus occurs as a baby's heart forms during pregnancy. There's often no clear cause. Genetics and environmental factors may play a role.
How the heart works
To understand more about truncus arteriosus, it may be helpful to know how the heart typically works.
The typical heart has four chambers. They are:
- The right upper chamber, also called the right atrium. This heart chamber receives oxygen-poor blood from the body.
- The right lower chamber, also called the right ventricle. This heart chamber pumps blood into the lungs through a large vessel called the pulmonary artery. The blood flows through the pulmonary artery into smaller vessels in the lungs where blood picks up oxygen.
- The left upper chamber, also called the left atrium. This heart chamber receives oxygen-rich blood from the lungs through vessels called pulmonary veins.
- The left lower chamber, also called the left ventricle. This chamber pumps the oxygen-rich blood to the body through the body's largest blood vessel, called the aorta.
A baby's heart before birth
The way the unborn baby's heart forms during pregnancy is complex. At some point, there is a single large blood vessel leading out of the heart. The vessel is called the truncus arteriosus. It usually splits in two as the unborn baby grows in the womb. One part becomes the lower end of the body's main artery, called the aorta. The other part becomes the lower part of the pulmonary artery.
But in some babies, the truncus arteriosus never splits. The wall separating the two lower heart chambers hasn't closed all the way. This results in a large hole between those chambers, called a ventricular septal defect.
Babies with truncus arteriosus also often have a problem with the heart valve that controls blood flow from the lower heart chambers to the single vessel. This valve may not close all the way when the heart relaxes. Blood can move the wrong way, back into the heart. This is called truncal valve regurgitation.
Risk factors
The exact cause of truncus arteriosus is unknown. But some things might increase the risk of a heart problem at birth. Risk factors include:
- Viral illness during pregnancy. Some infections can hurt a developing baby. For example, having German measles during pregnancy can cause changes in a baby's heart development. German measles also is called rubella.
- Poorly controlled diabetes during pregnancy. Careful control of your blood sugar before and during pregnancy can reduce the risk of heart problems in your baby. If you have diabetes, work with your healthcare professional to be sure blood sugar is well controlled before getting pregnant.
- Some medicines taken during pregnancy. Some medicines can cause heart problems and other health conditions in a baby. Tell your healthcare professional about all the medicines you take, including those bought without a prescription.
- Some chromosomal disorders. An extra or irregular chromosome increases the risk of truncus arteriosus. Examples are DiGeorge syndrome, also called 22q11.2 deletion syndrome, and velocardiofacial syndrome.
- Smoking during pregnancy. If you smoke, quit. Smoking during pregnancy increases the risk of heart conditions in your baby.
- Alcohol use. Drinking alcohol during pregnancy increases the risk of heart conditions and other health issues in a baby.
- Obesity. Obesity increases the risk of giving birth to a baby with a heart condition.
Complications
Truncus arteriosus causes severe problems with how blood flows through the lungs, heart and rest of the body.
Complications of truncus arteriosus in babies include:
- Breathing problems. Extra fluid and blood in the lungs can make it difficult to breathe.
- High blood pressure in the lungs, also called pulmonary hypertension. This condition causes the blood vessels in the lungs to narrow. It becomes hard for the heart to pump blood into the lungs.
- Enlargement of the heart. Pulmonary hypertension and increased blood flow strain the heart. The heart must work harder to pump blood. This causes the heart muscle to grow larger. The enlarged heart gradually weakens.
- Heart failure. In this condition, the heart cannot supply the body with enough blood. Too little oxygen and too much strain on the heart can lead to heart failure.
Infants who had their hearts successfully fixed with surgery may still have complications later in life. Possible complications are:
- Pulmonary hypertension that gets worse.
- Backward flow of blood through a heart valve, called regurgitation.
- Irregular heartbeats, called arrhythmias.
Common symptoms of these complications include:
- Dizziness.
- Feeling very fast, fluttering heartbeats.
- Feeling very tired.
- Shortness of breath when exercising.
- Swelling of the belly, legs or feet.
Truncus arteriosus in adults
In rare cases, some people born with truncus arteriosus can survive without heart surgery. They may live into adulthood. But those with the condition will almost certainly have heart failure and develop a complication called Eisenmenger syndrome. This syndrome is caused by permanent lung vessel damage. It results in a significant lack of blood flow to the lungs.
Prevention
Because the cause is unclear, it may not be possible to prevent truncus arteriosus. Getting good prenatal care is important. If you or someone in your family had a heart condition present at birth, talk to your healthcare professional before getting pregnant. You might need to see a genetic counselor and a heart doctor, called a cardiologist.
If you decide to get pregnant, taking these steps can help keep your baby healthy:
- Get recommended vaccinations. Some infections can be harmful to a developing baby. For example, having German measles — also called rubella —during pregnancy can cause changes in a baby's heart development. A blood test done before pregnancy can show if you're immune to rubella. A vaccine is available for those who aren't immune.
- Talk to your healthcare professional about your medicines. Check with your healthcare professional before taking any medicines if you're pregnant or thinking about getting pregnant. Many drugs aren't recommended for use during pregnancy because they can harm a developing baby.
- Take a folic acid supplement. Take a multivitamin with folic acid. Taking 400 micrograms of folic acid daily has been shown to reduce brain and spinal cord conditions in babies. It may help reduce the risk of heart conditions present at birth too.
- Control diabetes. If you have diabetes, ask your healthcare professional how to best manage the disease during pregnancy.
Nov. 21, 2024