Diagnosis
A thorough exam and proper diagnostic tests are needed for an accurate diagnosis. A misdiagnosed penicillin allergy may result in the use of improper or more expensive antibiotics.
Your healthcare professional conducts a physical exam and ask questions about your symptoms. Your health professional also may order tests. You may be referred to an allergy specialist, called an allergist, for these tests. Tests may include the following.
Skin tests
With a skin test, the allergist or nurse puts a small amount of the suspect penicillin in your skin with a tiny needle. A positive reaction to a test causes a discolored, itchy, raised bump.
A positive result means the likelihood of penicillin allergy is high. A negative test result usually means you're not at high risk of an allergy to penicillin. But a negative result is more difficult to understand because some kinds of medicine reactions cannot be detected with skin tests.
Graded challenge
If the diagnosis of a penicillin allergy is uncertain, a graded challenge may be recommended. With this procedure, you receive up to five doses of the suspect penicillin. The challenge starts with a small dose and increases to the desired dose. If you reach the desired dose with no reaction, your healthcare professional concludes that you aren't allergic to that type of penicillin. You will be able to take the antibiotic as prescribed.
If you are allergic to one type of penicillin, you may have to do a graded challenge with a type of penicillin or cephalosporin that's less likely to cause an allergic reaction. This would help your healthcare professional find an antibiotic that you can safely use.
During a graded challenge, you're carefully monitored. Supportive care services also are available to treat a reaction.
Treatment
Treatments for a penicillin allergy can be divided into two general strategies:
- Treatment for the current allergy symptoms.
- Treatment to lessen sensitivity to penicillin, called desensitization.
Treating current symptoms
The following treatments may be used for symptoms of an allergic reaction to penicillin:
- Withdrawal of the medicine. If your healthcare professional determines that you have or likely have a penicillin allergy, stopping the medicine is the first step in treatment.
- Antihistamines. You may be prescribed an antihistamine. You also may use an antihistamine that you can buy without a prescription. Antihistamines can block the immune system during an allergic reaction.
- Corticosteroids. Either oral or injected corticosteroids may be used to treat inflammation related to more-serious reactions.
- Treatment of anaphylaxis. Anaphylaxis requires an immediate treatment with medicine as well as hospital care to maintain blood pressure and support breathing.
Medicine desensitization
If there are no other suitable antibiotic treatment options available, your healthcare professional may recommend a treatment called drug desensitization. This allows you to take a course of penicillin to treat an infection. With this treatment, you receive a very small dose of the medicine. The dose gets larger every 15 to 30 minutes over the course of several hours or a few days. If you can reach the desired dose with no reaction, you can continue the treatment.
It's important to take the medicine as directed to maintain your tolerance to it during the entire course of treatment. If you need penicillin in the future, you will likely need to repeat the desensitization treatment.
You're carefully monitored during the treatment. Supportive care also is available to treat reactions. Desensitization is not always successful, and there is a risk of serious reactions.
Preparing for your appointment
Be prepared to answer questions, such as:
- What symptoms did you experience?
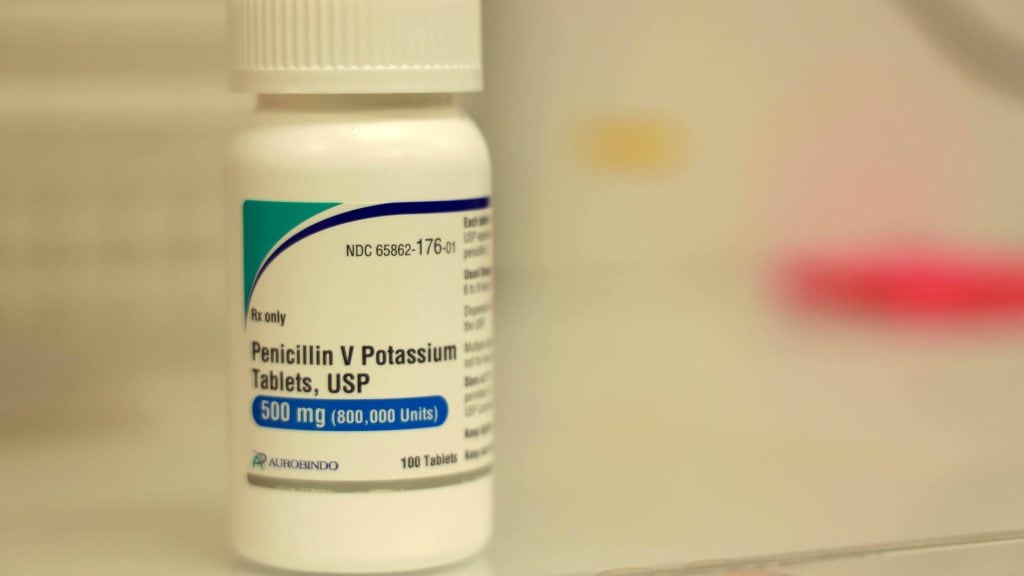
- What is the name of the penicillin or other antibiotic you were taking?
- Why were you prescribed the antibiotic?
- Have you had these symptoms in the past when you weren't taking this medicine?
- How long after taking penicillin did the symptoms begin?
- How long did the symptoms last?
- Have you stopped taking the medicine?
- What other medicines, herbal medicines, vitamins or other dietary supplements do you take?
- At what time of day do you take your other medicines or supplements?
- Have you increased the dosage of any regular medicine or supplement?
- Have you stopped taking your regular medicines or supplements?
- Did you take anything to treat your symptoms? If so, what was the effect?
- Have you had a reaction to any medicine in the past? If so, what medicine was it?
- Do you have hay fever, food allergy or other allergies?
- Is there a history of penicillin or other medicine allergies in your family?
You may want to take pictures of any condition, such as a rash or swelling, to show your healthcare professional. Pictures may help your healthcare professional if symptoms have gotten better by the time of your appointment.