Diagnosis
Screening tests and procedures used to detect and diagnose brain aneurysms include:
-
CT scan. This specialized X-ray is usually the first test used to assess for bleeding in the brain or another type of stroke. The test produces images that are 2D slices of the brain.
A CT angiogram can create detailed images of the arteries providing blood flow in the brain. The test involves injecting dye into the vein that makes it easier to observe blood flow. It also can detect the presence of an aneurysm.
-
Lumbar puncture, known as a spinal tap. If you've had a subarachnoid hemorrhage, there will most likely be red blood cells in the fluid surrounding your brain and spine. This fluid is called cerebrospinal fluid. If you have symptoms of a ruptured aneurysm but a CT scan doesn't show evidence of bleeding, a test of your cerebrospinal fluid can help make a diagnosis.
The procedure to draw cerebrospinal fluid from your back with a needle is called a lumbar puncture.
-
MRI. This imaging test uses a magnetic field and radio waves to create detailed images of the brain. These images may be either 2D or 3D images and can show if there's bleeding in the brain.
A type of MRI that captures images of the arteries in detail is called MR angiography. This type of MRI can detect the size, shape and location of an aneurysm.
-
Cerebral angiogram. During this procedure, a thin, flexible tube called a catheter is used. The catheter is inserted into an artery, usually in the groin or the wrist. The catheter threads past your heart to the arteries in your brain. A special dye injected into the catheter travels to arteries throughout your brain.
A series of X-rays can then reveal details about the conditions of your arteries and detect an aneurysm. A cerebral angiogram — also called a cerebral arteriogram — is usually used when other diagnostic tests don't provide enough information.

A doctor shares information about brain aneurysm diagnosis.
Screening for brain aneurysms
Screening for unruptured brain aneurysms is typically only used if you are at high risk. Talk to your healthcare professional about screening if you have:
- A family history of brain aneurysms or a hemorrhagic stroke. Particularly if two first-degree relatives — your parents, siblings or children — have had a brain aneurysm or hemorrhagic strokes.
- A condition that increases your risk of developing a brain aneurysm. These disorders include polycystic kidney disease, coarctation of the aorta or Ehlers-Danlos syndrome, among others.
Most aneurysms don't rupture. And for many people, an unruptured aneurysm never causes symptoms. But if the aneurysm ruptures, several factors may affect the outcome, which is known as the prognosis. They include:
- The person's age and health.
- Whether the person has other conditions.
- The size and location of the aneurysm.
- How much bleeding has happened.
- How much time passed before receiving medical care.
About 25% of people who experience a ruptured aneurysm die within 24 hours. Another 25% have complications that lead to death within six months.
More Information
Treatment
Repairing a ruptured aneurysm requires surgery or endovascular treatment. Endovascular treatment means an aneurysm is treated from inside the artery. You also may be given treatments to relieve symptoms.
If you have an unruptured aneurysm, talk with your healthcare professional about possible treatments. Talk about whether the risk of leaving the aneurysm alone is greater than the risk of treating the aneurysm.
Factors that your healthcare team considers before making treatment recommendations include:
- The aneurysm size, location and overall appearance of the aneurysm.
- Your age and general health.
- Family history of ruptured aneurysm.
- Conditions you were born with that increase the risk of a ruptured aneurysm.
Surgery

Mayo Clinic surgeons perform an endovascular procedure for brain aneurysm.
There are two common treatment options for repairing a ruptured brain aneurysm. For some people, these procedures may be considered to treat an unruptured aneurysm. However, the potential treatment risks may outweigh the potential benefits for some unruptured aneurysms.
Aneurysm clip
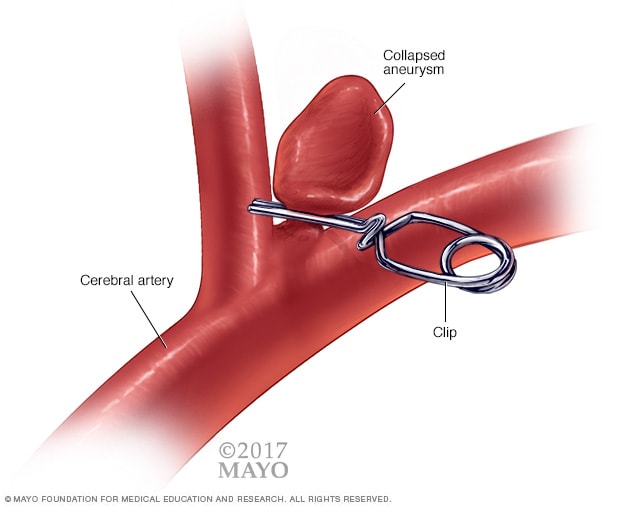
Aneurysm clip
A surgical procedure to treat brain aneurysms involves opening the skull, finding the affected artery and then placing a metal clip over the neck of the aneurysm.
Surgical clipping
Surgical clipping is a procedure to close off an aneurysm. The neurosurgeon removes a section of your skull to access the aneurysm. The neurosurgeon then locates the blood vessel that feeds the aneurysm. The surgeon places a tiny metal clip on the neck of the aneurysm to stop blood flow into it.
Surgical clipping can be very effective. Typically, aneurysms that are clipped don't return. The risks of surgical clipping include bleeding in the brain or loss of blood flow to the brain. These risks are low.
Recovery from surgical clipping usually takes about 4 to 6 weeks. When surgical clipping is done for an unruptured aneurysm, many people can leave the hospital a day or two after surgery. For those who have surgical clipping because of a ruptured aneurysm, the hospital stay is typically much longer as they recover from the aneurysm rupture.
Endovascular coiling
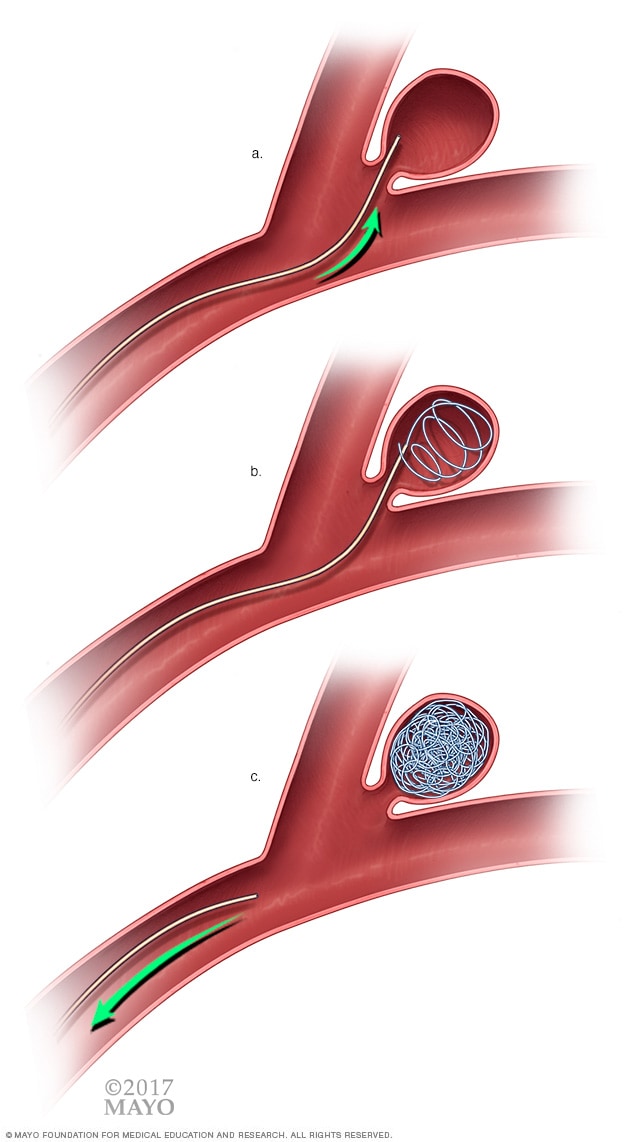
Endovascular coiling
With endovascular coiling, the surgeon feeds a soft, flexible wire into the aneurysm via a catheter. The wire coils inside the aneurysm and seals off the aneurysm from the artery.
Endovascular treatment
This is a less invasive procedure than surgical clipping, and it may be safer. Endovascular treatment involves accessing the aneurysm by threading a small plastic tube called a catheter through the artery. The catheter is moved into the brain arteries. Then coils may be placed.
- Endovascular coils. During this procedure, a neurosurgeon inserts the catheter into an artery, usually in the groin or wrist. Then the surgeon threads it through the body to the aneurysm. A tiny coil shaped like a spiral is placed inside the aneurysm. This prevents blood from flowing into the aneurysm. The coil also causes the blood that's in the aneurysm to clot.
- Endovascular stents. A stent is a small tube that may be used with an endovascular coil for some types of brain aneurysms. A stent can hold the coil in place.
Like surgical clipping, endovascular treatment carries the risk of bleeding in the brain or loss of blood flow to the brain. Also, there's a risk that the aneurysm may again appear over time. If that happens, the procedure may need to be repeated. You'll likely need follow-up imaging tests to be sure the aneurysm hasn't returned.
Flow diversion
Flow diversion is an endovascular treatment option for treatment of a brain aneurysm. The procedure involves placing a stent in the blood vessel to divert blood flow away from the aneurysm. The stent that's placed is called a flow diverter.
With less blood flow going to the aneurysm, there's less risk of rupture. It also allows the body to heal. The stent prompts the body to grow new cells that seal the aneurysm.
Flow diversion may be particularly useful in larger aneurysms that can't be treated with other options and in locations that are more difficult to treat with surgery or standard endovascular treatments.
Other procedures for ruptured aneurysms
Other procedures to treat ruptured aneurysms and complications of the rupture may include:
- Angioplasty. This is a procedure to expand a narrowed blood vessel in the brain caused by vasospasm. The procedure also can help prevent a stroke.
- Ventricular or lumbar draining catheters and shunt surgery can lessen pressure on the brain from a buildup of cerebrospinal fluid. A catheter may be placed in the spaces that are filled with fluid inside the brain. Or it can be placed in the area surrounding the brain and spinal cord. The catheter drains the excess fluid into an external bag or into the abdomen for more permanent drainage.
Medicines for ruptured brain aneurysms
Medicines may be used after a ruptured brain aneurysm to relieve symptoms and manage complications. Medicines may include:
- Pain relievers, such as acetaminophen (Tylenol, others), may be used to treat headache pain.
-
Calcium channel blockers prevent calcium from entering cells of the blood vessel walls. These medicines may lessen the risk of having symptoms from the narrowing of blood vessels, known as vasospasm. Vasospasm may be a complication of a ruptured aneurysm.
One of these medicines, nimodipine (Nymalize), has been shown to reduce the risk of delayed brain injury caused by insufficient blood flow. This can happen after subarachnoid hemorrhage from a ruptured aneurysm.
- Medicines to open blood vessels. A medicine can be given to dilate the blood vessels. This can be given through an IV in the arm or with a catheter directly into the arteries supplying the brain. This can help prevent a stroke by allowing the blood to flow freely. Blood vessels also can be expanded using medicines known as vasodilators.
- Anti-seizure medicines may be used to treat seizures related to a ruptured aneurysm. The medicines typically aren't given if a seizure hasn't happened.
Rehabilitative therapy may be used after a brain aneurysm ruptures. Damage to the brain from a subarachnoid hemorrhage may result in the need for physical, speech and occupational therapy to relearn skills.
Treating unruptured brain aneurysms
A surgical clip, an endovascular coil or a flow diverter can be used to seal off an unruptured brain aneurysm. This can help prevent a future rupture. However, the risk of rupture may be extremely low in some unruptured aneurysms, and the known risks of the procedures may outweigh the potential benefits.
A neurologist working with a neurosurgeon or interventional neuroradiologist can help you decide if treatment is right for you.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
If you have an unruptured brain aneurysm, you may lower the risk of rupture by making these lifestyle changes:
- Don't smoke cigarettes. If you smoke, talk to your healthcare professional. They can suggest strategies or a treatment program to help you quit.
- Manage your blood pressure if you have high blood pressure.
- Eat a healthy diet and exercise. Changes in diet and exercise can help lower blood pressure. Talk to your healthcare professional about changes that are right for you.
- Don't use alcohol in excess.
- Don't use recreational drugs such as cocaine, methamphetamine or others. If you do use these drugs and would like to quit, talk to your healthcare professional.
Coping and support
The Brain Aneurysm Foundation offers information on connecting with support groups in many states and in other countries.
Preparing for your appointment
If test results show you have a brain aneurysm, you'll need to talk with a specialist in brain and nervous system conditions. These specialists include neurologists, neurosurgeons and neuroradiologists.
Here's some information to help you get ready for your appointment.
What you can do
- Be aware of anything you need to do ahead of time. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you have, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down important personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements you're taking and the doses.
- Take a family member or friend along. It can be hard to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For unruptured brain aneurysms, some basic questions to ask include:
- What do you know about the size, location and overall appearance of the aneurysm?
- How likely is my aneurysm to rupture?
- What treatment do you recommend at this time? What are the risks of treatment?
- If treatment is not indicated currently, how often will I need to have follow-up scans for the aneurysm?
- What steps can I take to lower the risk of an aneurysm rupturing?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- Do you smoke cigarettes?
- How much alcohol do you drink?
- Do you use recreational drugs?
- Are you being treated for high blood pressure?
- Do you take your medicines as prescribed by your healthcare professional?
- Is there a history of brain aneurysm or brain aneurysm rupture in your family?
- What is your medical history?