نظرة عامة
الجراحة هي العلاج الأكثر شيوعًا لسرطان المستقيم. وتهدف الجراحة إلى استئصال الورم السرطاني وكمية كافية من الأنسجة المحيطة به لمحاولة علاج السرطان أو منعه من الانتشار، مع الحفاظ قدر الإمكان على الوظائف الطبيعية للأمعاء والمثانة.
يعتمد نوع الإجراء الطبي الموصى به على مدى انتشار الورم ومكانه في المستقيم. وفي بعض الأحيان قد تكون هناك حاجة إلى إجراء لتحويل مسار خروج البراز من الجسم، مثل فغر اللفائفي أو فَغر القولون.
إضافةً إلى الجراحة، قد يوصي فريق الرعاية الصحية بعلاجات أخرى، مثل العلاج الكيميائي أو العلاج الإشعاعي. ويمكن استخدام هذه العلاجات قبل الجراحة أو أثناءها أو بعدها. ويمكن استخدامها لتقليص حجم السرطان أو المساعدة في قتل أي خلايا سرطانية متبقية لم تُستأصل بالجراحة.
تشريح المستقيم
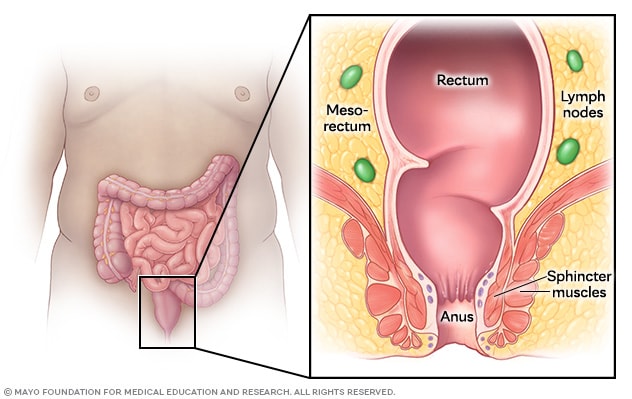
تشريح المستقيم
يشكل المستقيم والشرج الجزء الأخير من الجهاز الهضمي. يخزن المستقيم البراز إلى أن يخرج من الجسم عبر فتحة الشرج. وتساعد عضلات المَصَرّة على التحكم في حركة الأمعاء. المستقيم محاط بأنسجة دهنية تُسمى مسراق المستقيم، وتحتوي على أوعية دموية وعُقَد لمفية. وتشكل العُقَد اللمفية جزءًا من جهاز الجسم المناعي.
الأنواع
توجد أنواع كثيرة ومختلفة من جراحات سرطان المستقيم. عند التوصية بالجراحة، يأخذ فريق الرعاية الصحية في الحسبان مكانَ السرطان في المستقيم، وما إذا كان السرطان قد انتشر خارج المستقيم.
تتضمن أنواع جراحة سرطان المستقيم:
إجراءات الاستئصال الموضعي
يُستخدم الاستئصال الموضعي عادةً عندما يكون سرطان المستقيم في مرحلة مبكرة ولم ينتشر إلى العُقَد اللمفية. يُزيل هذا النوع من الجراحة الورم من خلال فتحة الشرج دون فتح أي شقوق في البطن. عادةً يكون التعافي من هذا الإجراء الطبي أسرع من الإجراءات الطبية المماثلة الأخرى.
ومع ذلك، لا يُزيل الاستئصال الموضعي العُقَد اللمفية أو الأنسجة الأعمق. قد لا يكون هذا الإجراء كافيًا إذا كان السرطان قد نما بشكل عميق في جدار المستقيم، أو لم يُزَل بالكامل، أو أظهر مؤشرات على انتشاره إلى العُقَد اللمفية أو الأوعية الدموية. في تلك الحالات، قد تكون هناك حاجة إلى علاج إضافي، مثل العلاج الإشعاعي أو العلاج الكيميائي. في بعض الأحيان، قد يُوصى بإجراء جراحة أكبر، بناءً على نوع السرطان وموقعه.
تتضمن أنواع الاستئصال الموضعي:
- الاستئصال عبر الشرج (TAE). يَستخدم أسلوب الاستئصال عبر الشرج أدوات بسيطة لاستئصال السرطان من خلال فتحة الشرج. ويُجرى في أغلب الأحيان كإجراء دون مبيت في المستشفى.
- الجراحة طفيفة التوغل عبر الشرج (TAMIS). تَستخدم الجراحة طفيفة التوغل عبر الشرج أدوات تنظير البطن من خلال منفذ ليّن يُدخَل في فتحة الشرج. ويمكن أيضًا إجراؤها روبوتيًا لتحسين التحكم في الأماكن الضيقة. يُنفَخ المستقيم بالغاز لتوفير مساحة للجراح لإجراء الجراحة. وتعد الجراحة طفيفة التوغل عبر الشرج خيارًا مرنًا وأوفر تكلفة لعلاج السرطان في مراحله المبكرة.
- قَطع المخاطية بالتنظير (EMR) والتشريح تحت المخاطي بالتنظير الداخلي (ESD). يُستخدم قَطع المخاطية بالتنظير والتشريح تحت المخاطي بالتنظير الداخلي لإزالة السلائل، وخصوصًا تلك التي تقتصر على الطبقات الداخلية من جدار المستقيم. يُستخدم قَطع المخاطية بالتنظير عادةً لإزالة الأورام من الطبقة العليا، بينما يَسمح التشريح تحت المخاطي بالتنظير الداخلي بتشريح أعمق في الأنسجة. يُستخدم التشريح تحت المخاطي بالتنظير الداخلي في حال السرطانات الأكبر حجمًا أو الأكثر تعقيدًا. ويمكن استخدام هذه التقنيات أحيانًا لاستئصال السرطان في مراحله المبكرة.
بعد الاستئصال الموضعي لسرطان المستقيم، تُعد الفحوصات المنتظمة أمرًا أساسيًا لاكتشاف أي تكرار للإصابة بالسرطان في وقت مبكر.
الاستئصال مع الحفاظ على المَصَرّة
تُزيل هذه الجراحات السرطان والأنسجة القريبة منه، ولكنها تحاول الحفاظ على العضلات التي تتحكم في حركة الأمعاء، والتي تسمى العضلة الشرجية العاصرة (المَصَرّة الشرجية). قد تتطلب هذه الجراحات إجراء فغر مؤقت أو دائم، مثل فغر اللفائفي أو فغر القولون، الذي يتضمن فتح فتحة جراحية في البطن لمرور البراز.
- الاستئصال الكُلي لمسراق المستقيم (TME). الاستئصال الكُلي لمسراق المستقيم هو الإجراء الجراحي القياسي الأبرز لعلاج سرطان المستقيم. يتضمن هذا الإجراء فتح شق في البطن لإزالة الجزء المصاب من المستقيم مع الأنسجة الدهنية المحيطة به، التي تسمى مسراق المستقيم، والعُقَد اللمفية. يحقق الاستئصال الكُلي لمسراق المستقيم نتائج ممتازة في السيطرة على السرطان والبقاء على قيد الحياة، إلا أن مرحلة التعافي قد تنطوي على اضطرابات في الأمعاء وخلل وظيفي جنسي. ويتعافى معظم الأشخاص خلال ثلاثة إلى ستة أسابيع.
- الاستئصال الكلي لمسراق المستقيم عبر فتحة الشرج (taTME). هذا الإجراء الطبي طريقة جديدة لإجراء الاستئصال الكُلي لمسراق المستقيم من خلال فتحة الشرج، بدلاً من فتح شقوق في البطن مثل الاستئصال الكُلي لمسراق المستقيم التقليدي. قد يسمح الاستئصال الكلي لمسراق المستقيم عبر فتحة الشرج بإزالة الورم بشكل أسهل من خلال فتحة الشرج، خصوصًا عندما يكون السرطان موجودًا في أسفل المستقيم ويصعب الوصول إليه من خلال البطن.
-
الاستئصال الأمامي المنخفض (LAR). الاستئصال الأمامي المنخفض جراحة للحفاظ على العضلة العاصرة (المَصَرّة) في حال الإصابة بسرطان المستقيم في الجزء الأوسط إلى الجزء العلوي منه. ويتضمن هذا الإجراء إزالة السرطان والأنسجة المجاورة والعُقَد اللمفية، ثم يُعاد توصيل القولون بالمستقيم، ومن ثَم لا تكون هناك حاجة عادةً لإجراء فغر القولون الدائم. ومع ذلك، يلزم إجراء فغر اللفائفي المؤقت أحيانًا. قد يستغرق التعافي من ثلاثة إلى ستة أسابيع.
في بعض الأحيان، عندما يكون السرطان قريبًا جدًا من فتحة الشرج، يربط الجراح القولون مباشرةً بفتحة الشرج، بخياطته يدويًا، للمساعدة في تجنب فغر القولون الدائم.
-
استئصال المستقيم والقولون. يستأصل هذا الإجراء الطبي القولون والمستقيم. يمكن استخدام استئصال القولون والمستقيم لعلاج سرطان المستقيم متعدد البؤر أو المتكرر، أو المرتبط بمتلازمات وراثية مثل داء السلائل الورمي الغُدّي العائلي (FAP)، أو حالات أخرى مثل التهاب القولون التقرحي أو داء كرون.
بعد استئصال القولون والمستقيم، قد يُنشئ الجراحون جيبًا من نهاية الأمعاء الدقيقة ويوصلونه بفتحة الشرج. يسمح هذا الإجراء الطبي بحركة الأمعاء والتبرُّز دون الحاجة إلى فغر دائم. ويُعرف هذا باسم استئصال المستقيم والقولون الكلي مع مفاغرة الجيبة اللفائفية الشرجية (TPC-EI). استئصال المستقيم والقولون الكلي مع مفاغرة الجيبة اللفائفية الشرجية المعروف أيضًا باسم جراحة المفاغرة اللفائفية الشرجية هو إجراء للحفاظ على العضلة العاصرة. وتهدف جراحة المفاغرة اللفائفية الشرجية إلى تجنب الحاجة إلى وجود فتحة دائمة في جدار البطن لإخراج البراز.
يوجد نوع آخر من استئصال المستقيم والقولون يُعرف باسم استئصال المستقيم والقولون الكلي مع فغر اللفائفي الطرفي. قد يُجرى استئصال المستقيم والقولون الكلي مع فغر اللفائفي الطرفي إذا كانت جراحة المفاغرة اللفائفية الشرجية غير ممكنة أو إذا كانت قدرة المَصرة الشرجية على أداء وظائفها ضعيفة. وفي هذا الإجراء الطبي، يُجرى توصيل الأمعاء الدقيقة بفتحة دائمة في البطن للسماح بخروج الفضلات من الجسم.
-
استئصال القولون. يؤدي استئصال القولون إلى إزالة القولون بالكامل أو جزء منه. يمكن إجراء ذلك إذا كان السرطان يتضمن المستقيم والقولون معًا، أو إذا كان لدى شخص ما حالة مرَضية ذات احتمال كبير للتعرض للإصابة بسرطان المستقيم، مثل داء السلائل الورمي الغُدّي العائلي أو متلازمة لينش. بعد إزالة الجزء المصاب من القولون، يُعاد توصيل الجزء المتبقي من الأمعاء. وبعدها يغادر البراز الجسم كما كان من قبل.
في حال استئصال القولون بأكمله، فقد يربط الجراح الجزء المتبقي من القولون أو الأمعاء الدقيقة بفتحة تُفتح في البطن. ويسمح هذا بخروج الفضلات من الجسم من خلال فتحة تسمى الفغرة. يُسمى إجراء ربط القولون بالفغرة بفغر القولون. ويُسمى إجراء ربط الأمعاء الدقيقة بالفغرة بالفغر اللفائفي.
الاستئصال دون الحفاظ على المَصَرّة
في بعض الأحيان يكون السرطان في مكان منخفض جدًا أو قريبًا جدًا من عضلات المَصرة الشرجية. عندما يحدث هذا، يجب على الجراح إزالة فتحة الشرج والمستقيم. ويحتاج الجراح أيضًا إلى فتح فتحة دائمة في البطن لمرور البراز، وتسمى فغر القولون أو فغر اللفائفي.
-
الاستئصال البطني العجاني. يُستخدم الاستئصال البطني العجاني عندما يكون السرطان في الجزء السفلي من المستقيم ولا يمكن الحفاظ على المَصَرّة. يُستأصل الجزء السفلي من القولون والمستقيم وفتحة الشرج والأنسجة المحيطة في هذا الإجراء الطبي. ويتبع ذلك إجراء فغر يُسمى فغر القولون. قد يستغرق التعافي من ثلاثة إلى ستة أسابيع.
بالنسبة إلى الرجال، قد يُسبب الاستئصال البطني العجاني مشكلات جنسية، مثل صعوبة الانتصاب أو صعوبة الوصول إلى النشوة الجنسية. وقد تتأثر الخصوبة أيضًا. أما بالنسبة إلى النساء، فقد يُسبب الاستئصال البطني العجاني زيادة الألم خلال ممارسة الجنس وانخفاض التزليق وانخفاض الإثارة.
- استئصال أحشاء الحوض. جراحة كبرى يُستأصل فيها المستقيم والأعضاء المجاورة، مثل المثانة أو الرحم أو البروستاتا، وأحيانًا العظام الموجودة في قاعدة العمود الفقري، التي تُسمى عظم العجُز. يُجرى استئصال أحشاء الحوض عندما يكون السرطان قد انتشر وصولاً إلى هذه المناطق.
فغر القولون أو فغر اللفائفي
بناءً على الإجراء الطبي، قد تكون هناك حاجة إلى فغر مؤقت أو دائم بعد الجراحة. وتشمل أنواع الفغر:
- فغر القولون. في إجراء فغر القولون، يُخرج طرف القولون من خلال جدار البطن لإنشاء فغر. ويمر البراز عبر الفغرة إلى كيس يوضع خارج الجسم. يمكن أن يكون فغر القولون دائمًا أو مؤقتًا بناءً على الجراحة.
- فغر اللفائفي. يُشبه إجراء فغر اللفائفي إجراءَ فغر القولون، ولكنه يستخدم طرف الأمعاء الدقيقة، والتي تسمى اللفائفي، بدلاً من القولون. ويُستخدم غالبًا عند استئصال القولون بأكمله أو عندما يحتاج المستقيم إلى وقت للتعافي بعد الجراحة.
لماذا يتم ذلك؟
الجراحة هي العلاج الأساسي لمعظم الأشخاص المصابين بسرطان المستقيم. وتتضمن إزالة السرطان وجزء صغير من النسيج السليم المحيط به، ويُعرف باسم الحواف. يستأصل الجراح كذلك العُقَد اللمفية المجاورة لأن السرطان يمكن أن ينتشر إليها أولاً. ويساعد ذلك على زيادة فرصة الشفاء من السرطان إلى أقصى حد.
المخاطر
تنطوي جراحة سرطان المستقيم على خطر التعرض لحدوث مضاعفات خطيرة. قد تساعد الإجراءات طفيفة التوغل، مثل الجراحة بالمنظار والجراحة الروبوتية، على التعافي بشكل أسرع والحد من حدوث مضاعفات. إلا أن هذا النوع من الجراحة ليس خيارًا علاجيًا مناسبًا لجميع المرضى.
يتوقف خطر التعرض لمضاعفات على الصحة العامة للمريض ونوع الجراحة التي يخضع لها والأسلوب الذي يتبعه الجرَّاح لتنفيذ العملية.
قد تشمل مضاعفات جراحة سرطان المستقيم بوجه عام:
- النزف.
- الجلطات الدموية.
- العَدوى
- مواجهة صعوبة في التحكم في التبرز، وتُسمى متلازمة الاستئصال الأمامي السفلي (LARS).
- الحاجة إلى التبول بشكل متكرر أو مُلِح.
- تسرب البول أو صعوبة إفراغ المثانة.
- الخلل الوظيفي الجنسي، مثل صعوبة الانتصاب أو الحفاظ على الانتصاب لدى الرجال، أو الشعور بعدم الارتياح أثناء العلاقة الجنسية لدى النساء.
- الإرهاق أو الضعف المستمر.
- تكوُّن أنسجة ندبية بعد الجراحة -تُسمى الالتصاقات- يمكن أن تُسبب انسدادًا في الأمعاء.
- تسرّب في موضع وصل أطراف الأمعاء السليمة بعد الجراحة، أو ما يُعرف بالمفاغرة.
- الوفاة في حالات نادرة.
قد تحدث بعض هذه المضاعفات، مثل الخلل الوظيفي الجنسي أو البولي، بسبب تأثر الأعصاب في الحوض أثناء الجراحة. ويختلف الخطر باختلاف نوع العملية الجراحية ومكان الورم وما إذا كنت قد خضعت لعلاج إشعاعي أو كيميائي قبل الجراحة.
كيف تستعد؟
ناقش الإجراء الطبي مع جراح سرطان المستقيم
قبل إجراء الجراحة، سوف تُقابل جراح سرطان المستقيم الذي يمكنه أن يشرح ما يمكن توقعه من الجراحة. استعد لهذا الاجتماع بإعداد قائمة بالأسئلة التي ستطرحها.
الأسئلة التي يمكن طرحها عن الجراحة:
- ما الخيارات المتاحة أمامي لجراحة سرطان المستقيم؟
- هل توصي بإجراء عملية جراحية مفتوحة أم طفيفة التوغل؟
- هل سأحتاج إلى إجراء الفغر مثل فغر القولون أو فغر اللفائفي؟ وفي تلك الحالة، هل سيكون هذا مؤقتًا أم دائمًا؟
- هل سأحتاج أيضًا إلى الخضوع لأنواع أخرى من العلاج، مثل العلاج الكيميائي أو الإشعاعي؟
الأسئلة التي يمكن طرحها عن المخاطر والتعافي:
- ما المخاطر المرتبطة بهذه الجراحة؟
- ما الخيارات المتاحة لإدارة الألم؟
- كم من الوقت سأقضي في المستشفى؟
- كم من الوقت سأحتاج للتعافي؟
- متى يمكنني تناوُل الطعام والشراب بعد الجراحة؟
- ما نوع النظام الغذائي الذي يجب أن أتبعه أثناء فترة التعافي؟ وما مدة ذلك؟
- هل يجب عليّ تقليل نشاطي بعد الجراحة؟
- متى أستطيع العودة للعمل؟
الأسئلة التي يمكن طرحها عن إجراء الفغر:
- كيف تبدو الفغرة وكيف يمكنني العناية بها؟
- كم مرة أحتاج إلى تغيير كيس الفغر؟
- هل يمكنني اتباع نظامي الغذائي المعتاد بعد إجراء الفغر؟
- كيف سيؤثر الفغر في حياتي اليومية وروتيني، مثل الأنشطة البدنية أو العلاقة الحميمية؟
- ما المضاعفات أو المخاطر المحتملة المرتبطة بالفغر؟
- كيف يمكنني التحكم في الرائحة والتسرب من كيس الفغر؟
- ما الدعم والموارد المتاحة للمساعدة في التعامل مع الفغر؟
اتَّبع تعليمات فريق الرعاية الصحية
في الأيام التي تسبق هذا الإجراء الطبي، قد يوصي فريق الرعاية الصحية بما يلي:
- التوقف عن تناول أدوية معينة. قد تزيد بعض الأدوية من احتمال حدوث مضاعفات أثناء الجراحة، لذلك قد يطلب فريق الرعاية التوقف عن استخدامها قبل موعد الإجراء الجراحي.
- الصوم قبل الجراحة. قد يُطلب الامتناع عن تناوُل الطعام والشراب قبل الإجراء الطبي بعدة ساعات أو يوم كامل. وسيقدّم فريق الرعاية التعليمات المحددة بهذا الشأن.
- شُرب محلول لتنظيف الأمعاء. قد يصف الطبيب محلولاً مُليّنًا يمكنك خلطه بالماء في المنزل، ويُشرب هذا المحلول على مدى عدة ساعات. ينبغي اتباع تعليمات فريق الرعاية، إذ يُسبب هذا المحلول الإسهال، للمساعدة في إفراغ القولون والمستقيم. وقد يوصي فريق الرعاية باستخدام الحقن الشرجية أيضًا.
- تناوُل مضادات حيوية. قد يصف الطبيب مضادات حيوية لتثبيط نشاط البكتيريا الموجودة بشكل طبيعي في الأمعاء والمساعدة في الوقاية من العَدوى.
- الإقلاع عن التدخين. يجعل التدخين من الصعب على الجسم التعافي بعد الجراحة. لكن الإقلاع عن التدخين قبل الخضوع للجراحة قد يساعد في تعجيل التعافي ويقلل من حدوث المضاعفات.
- المحافظة على النشاط البدني. يمكن أن تُعزز الأنشطة البدنية قبل جراحة سرطان المستقيم التعافي والنتائج بوجه عام. وتساعد كذلك في تحسين صحة القلب والأوعية الدموية وقوة العضلات والصحة العقلية عمومًا ما قد يسهم في الحد من حدوث مضاعفات أثناء الجراحة وتعزيز سرعة التعافي بعدها.
التخطيط للإقامة في المستشفى
من المرجح أن تقضي بضعة أيام على الأقل في المستشفى بعد إجراء الجراحة. وتعتمد مدة بقائك على حالتك. ولهذا، ينبغي الترتيب مع شخص آخر ليتولى مسؤولياتك في المنزل والعمل. فكر مسبقًا في الأغراض التي قد تفضل إحضارها معك أثناء تعافيك في المستشفى.
تتضمن الأغراض التي يوصى بحزمها:
- رداءً وخفَّين.
- أدوات العناية الشخصية مثل فرشاة ومعجون الأسنان، ومستلزمات الحلاقة، عند الحاجة.
- ملابس مريحة لارتدائها عند العودة إلى المنزل.
- أغراض لممارسة أنشطة تملأ فيها وقتك، كالألعاب وقراءة الكتب أو المجلات.
ما يمكن أن تتوقعه
أثناء الإجراء الطبي
يعتمد ما يحدث أثناء الجراحة على نوع الإجراء المحدد. وبشكل عام، يمكن توقع ما يلي:
- التحضير للجراحة. يصحب أعضاء فريق الرعاية الصحية المريض إلى غرفة التحضير لقياس ضغط الدم ومتابعة معدل تنفسه. وقد يتلقى مضادًا حيويًا بالحَقن في أحد أوردة الذراع للوقاية من العَدوى. وقد يتلقى أيضًا دواءً للوقاية من الجلطات الدموية.
- التخدير. يصحب أعضاء فريق الرعاية الصحية المريض إلى غرفة العمليات حيث يستلقي على طاولة الجراحة. ويخضع المريض لتخدير عام يجعله في حال شبيهة بالنوم حتى لا يشعر بأي شيء أثناء العملية. وبمجرد أن ينام المريض وتفقد الوعي نتيجة للتخدير، يبدأ الجراح في إجراء الجراحة.
- استئصال السرطان. يستأصل الجرّاح السرطان والمستقيم بالكامل أو جزءًا منه. وفي معظم الحالات، تُستأصل أيضًا عينة من العُقَد اللمفية القريبة للتحقق مما إذا كان السرطان قد انتشر. يعتمد النهج المتبع على موقع الورم ومرحلته:
- في حالات السرطان في مراحله المبكرة، قد يستخدم الجراح تقنية الاستئصال الموضعي عبر فتحة الشرج، دون إجراء شقوق في البطن.
- وفي حالات السرطان الأكثر تقدمًا، قد يُجري الجراح قطعًا أماميًا منخفضًا (LAR) أو استئصالاً بطنيًا عجانيًا (APR). يتطلب كل من هذه الإجراءات فتح شقوق في البطن. يمكن إجراء هذه الإجراءات الطبية باستخدام تقنيات الجراحة المفتوحة أو التقنيات طفيفة التوغل، مثل الجراحة بتنظير البطن أو الجراحة الروبوتية.
- إعادة التوصيل أو الفغر. يُعيد الجراح توصيل الأجزاء المتبقية من الأمعاء إن أمكن للسماح بحركات الأمعاء الطبيعية. إذا كانت المنطقة تحتاج إلى وقت للالتئام أو إذا لم تكن إعادة التوصيل ممكنة، فقد يحتاج المريض إلى فغر مؤقت أو دائم. يُنشئ إجراء الفغر فتحة في جدار البطن تُسمّى الفغرة. ويسمح هذا للبراز بمغادرة الجسم من خلال كيس متصل بالفغرة.
بعد الإجراء الطبي
بعد الجراحة، ستُنقل إلى غرفة الإفاقة كي تُراقَب عن كثب بينما يزول مفعول التخدير. وبمجرد أن تستقر حالتك، ستُنقل إلى غرفتك في المستشفى لبدء مرحلة التعافي.
- استعادة وظائف الأمعاء الطبيعية. من المرجح أن تبقى في المستشفى حتى تتمكن من تناوُل الطعام والشراب مرة أخرى وتبدأ وظائف الأمعاء الطبيعية في العودة. وقد يستغرق ذلك عدة أيام. قد تُنصح بالبدء في اتباع نظام غذائي عادي خلال 24 ساعة بعد الجراحة. ويمكن أن يفيدك تناوُل لقيمات صغيرة ومضغها جيدًا والتوقف بين اللقيمات. يمكن أن يساعد تناوُل الطعام مبكرًا على بدء الأمعائك عملها بشكل أسرع.
- الأنشطة البدنية. من المرجح أن تُنصَح بالمشي في اليوم الأول بعد الجراحة. ترتبط ممارسة النشاط البدني بشكل فوري بالتعافي بشكل أسرع وحدوث مضاعفات أقل.
- العناية بالجروح. سيُعلّمك فريق الرعاية الصحية كيفية العناية بالشق الجراحي والتعامل مع أي أنابيب تصريف في موضع الجراحة. يمكن لأعضاء الفريق أيضًا تقديم تعليمات حول النظام الغذائي والنشاط البدني ومؤشرات المضاعفات التي يجب الانتباه لها.
- العناية بالفغر. إذا كانت الجراحة تتضمن فغر القولون أو فغر اللفائفي، فيمكن للممرضة أن تُعلِّمك كيفية العناية بالفغرة وتغيير كيس الفغر. بعض عمليات الفغر مؤقتة ويمكن عكسها بعد شفاء الأمعاء، وعادةً خلال مدة من 8 أسابيع إلى 12 أسبوعًا. وبعضها الآخر دائم، ويعتمد ذلك على نوع الجراحة وموقعها.
- استعادة الوظائف. قد تتغير عادات التغوط بعد جراحة المستقيم. يُصاب بعض الأشخاص بالرغبة الملحة في التغوط أو زيادة وتيرته أو السلَس. وتُعرف هذه الأعراض باسم متلازمة الاستئصال الأمامي السفلي (LARS). قد تتحسن أعراض متلازمة الاستئصال الأمامي السفلي مع مرور الوقت، خصوصًا مع إجراء تغييرات في النظام الغذائي وممارسة تمارين القاع الحوضي. في حال إجراء مفاغرة منخفضة جدًا أو إنشاء وصلة مستقيمة دون إنشاء جيب، فقد يستغرق استقرار وظيفة الأمعاء وقتًا أطول.
النتائج
بعد جراحة سرطان المستقيم، يراجع فريق الرعاية النتائج المرَضية للأنسجة التي استُؤصلت أثناء الجراحة. وتساعد هذه النتائج على تحديد ما إذا كانت هناك حاجة إلى علاج إضافي وخطة الرعاية التفقدية.
إذا أظهرت النتائج عدم وجود أي مؤشرات لبقاء السرطان، فقد يوصي فريق الرعاية باتباع نهج "المراقبة والانتظار" مع تحديد زيارات تفقدية منتظمة وإجراء اختبارات تصويرية. أمَّا إذا وُجدت خلايا سرطانية بالقرب من الحواف أو في العُقَد اللمفية، فقد يُوصى بعلاج إضافي مثل العلاج الكيميائي أو الإشعاعي.
قد يتعرض بعض الأشخاص لآثار طويلة الأجل من العلاج، مثل تغيُّرات في وظيفة الأمعاء أو المثانة، أو الخلل الوظيفي الجنسي، أو الإرهاق. وهذه أمور شائعة ويمكن علاجها. يمكن لفريق الرعاية أن يُحيلك إلى اختصاصيين مثل اختصاصيي معالجة القاع الحوضي، أو أطباء المسالك البولية، أو الاستشاريين للمساعدة في معالجة هذه الأمور.
الرعاية التفقدية
تُحدَّد لمعظم الأشخاص مواعيد زيارات تفقدية منتظمة لمدة لا تقل عن خمس سنوات. وقد تتضمن ما يلي:
- فحوصًا بدنية واختبارات دم كل ثلاثة إلى ستة أشهر خلال أول عامين، ثم كل ستة أشهر حتى مرور خمس سنوات.
- فحوصًا تصويرية مرة سنويًا أو بوتيرة أكبر إن دعت الحاجة.
- تنظير القولون بعد عام واحد من الجراحة، ثم بعد ثلاث سنوات، ثم كل خمس سنوات إذا لم تُكتشف أي مشكلات.