May 22, 2021
Overactive bladder is a relatively common condition: It impacts up to 30% of adults and can have a significant detrimental effect on quality of life. There are myriad treatments for overactive bladder, including behavioral, pharmacological and procedural strategies. However, there is a lack of knowledge regarding treatment patterns and progression among the various treatment options.
Leveraging an administrative claims database, researchers at Mayo Clinic in Rochester, Minnesota, led by Brian J. Linder, M.D., and Elizabeth B. Habermann, Ph.D., sought to evaluate longitudinal treatment patterns for women with overactive bladder who were privately insured. These treatment patterns included prescription filling, specialist referral, physical therapy and third line therapy use. The study was published in Female Pelvic Medicine & Reconstructive Surgery in 2021.
The researchers evaluated women 18 and older with a new overactive bladder diagnosis from January 1, 2007, to June 30, 2017. Exclusion criteria included:
- Neurogenic bladder or neurogenic etiology related to voiding dysfunction
- Pregnancy
- Prior overactive bladder diagnosis
- Anticholinergic or beta-3 agonist medication use in previous three months
- Any break in enrollment during the 12-month period
With these criteria, the researchers identified 60,246 patients for the cohort, with a median follow-up of 2.6 years. Of the participants, 37% were treated with anticholinergic medications, 4.9% were treated with beta-3 agonists, and 7.2% were treated with topical vaginal estrogen.
Sacral nerve modulation device
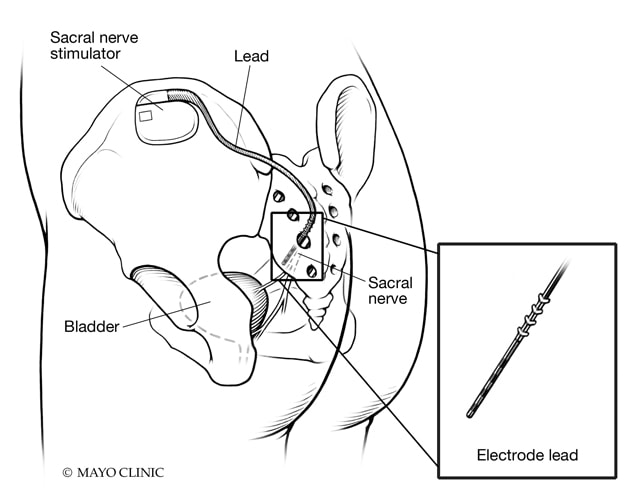
Sacral nerve modulation device
Schematic of a sacral nerve modulation device with placement in a sacral foramen.
Sacral nerve stimulator electrode placement
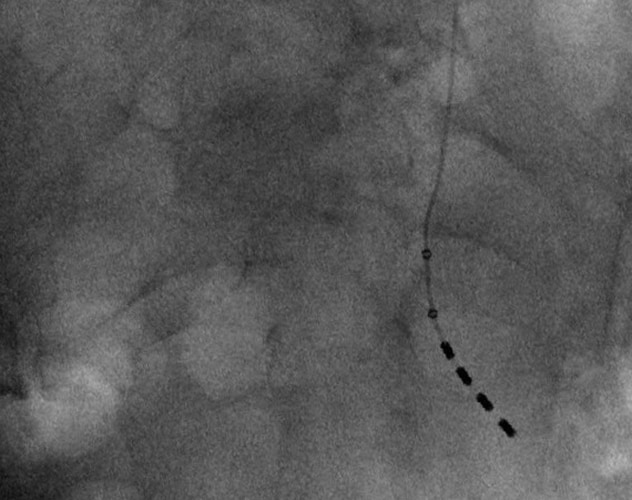
Sacral nerve stimulator electrode placement
Anterior-posterior view of appropriate placement of a sacral nerve stimulator electrode.
Sacral nerve stimulator placement
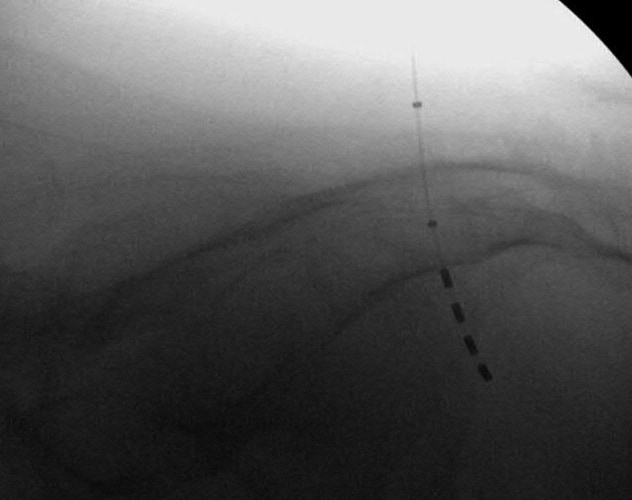
Sacral nerve stimulator placement
Lateral view of successful placement of a sacral nerve stimulator.
Further, 1.8% underwent pelvic floor physical therapy, 26% were referred to a specialist, and ultimately 2% underwent third line therapy. Third line therapies include onabotulinumtoxinA injection, percutaneous tibial nerve stimulation or sacral neuromodulation.
Changes in treatment over time were evaluated using the Cochran-Armitage test, and association of variables with risk of progression to third line therapy was assessed using multivariable logistic regression, reported as odds ratios and confidence intervals. Statistical significance was considered for p < 0.05.
Trends over time in the management of overactive bladder
When assessed over the study period, there was a significant trend toward increased use of beta-3 agonists (0.4% to 10.5%) and a decline in use of anticholinergic medication (39.6% to 32.4%). Beta-3 agonists also had a significantly longer time to discontinuation and increased medication use beyond last follow-up, in comparison with anticholinergics.
Use of third line therapies increased significantly (from 1.1% to 2.2%) over the study time frame. Of those patients who were treated with a third line therapy, the proportion of sacral neuromodulation decreased consistently and onabotulinumtoxinA increased. In the final year of the study (2017), the breakdown of third line treatments showed that onabotulinumtoxinA represented 37.8% of cases, sacral neuromodulation represented 36% of cases and tibial nerve stimulation represented 31.5% of cases. Referral to a specialist in urology or obstetrics and gynecology was associated with a significantly increased rate of third line therapy use.
Future directions
Dr. Linder notes: "Referral to specialists may close a gap in care for women who do not have success with oral therapies for overactive bladder. Increased education around treatment options, in the event that oral medications do not control symptoms or cause bothersome side effects, will help ensure patients can seek further relief from their symptoms.
"Overall, in our study there was a low rate of utilization for third line therapies, though the data shows this is increasing over time. Use of these therapies was more likely among patients seen by a specialist. Anecdotally, for many women, we have seen significant improvements in overactive bladder symptoms with third line therapies when an oral medication wasn't the solution for them."
For more information
Linder BJ, et al. National patterns of filled prescriptions and third-line treatment utilization for privately insured women with overactive bladder. Female Pelvic Medicine & Reconstructive Surgery. 2021;27:e261.