Sept. 29, 2016
Pediatric and adult structural interventional cardiologists have teamed up at Mayo Clinic in Rochester, Minnesota, to provide advanced levels of care for patients with bioprosthetic systemic atrioventricular (AV) valve dysfunction. Congenital and transcatheter valve implantation expertise, in combination with a team approach, has led to significant advances in and contributions to this field.
Utilizing techniques learned from percutaneous valve implantation procedures, Mayo Clinic physicians have been instrumental in advancing the treatment of patients who have previously undergone surgery to replace the mitral or tricuspid valve with a tissue bioprosthesis, and have published some of the earliest reports and publications on this type of approach. Existing dysfunctional bioprosthetic valves can be "replaced" with transcatheter valves.
Tricuspid valve
Mayo Clinic has a large referral population of patients with tricuspid valve (TV) abnormalities, such as Ebstein anomaly. Tricuspid valve surgical replacement is often necessary as part of treatment.
"Bioprosthetic tissue valves implanted surgically will eventually become dysfunctional with regurgitation, stenosis or combined dysfunction," according to Nathaniel W. Taggart, M.D., a pediatric cardiologist at Mayo Clinic in Rochester, Minnesota. "If a patient can be treated with transcatheter valve-in-valve (VIV) therapy, that approach is preferred over open-heart surgery and an additional median sternotomy."
Tricuspid valve-in-valve implantation
Tricuspid valve-in-valve implantation
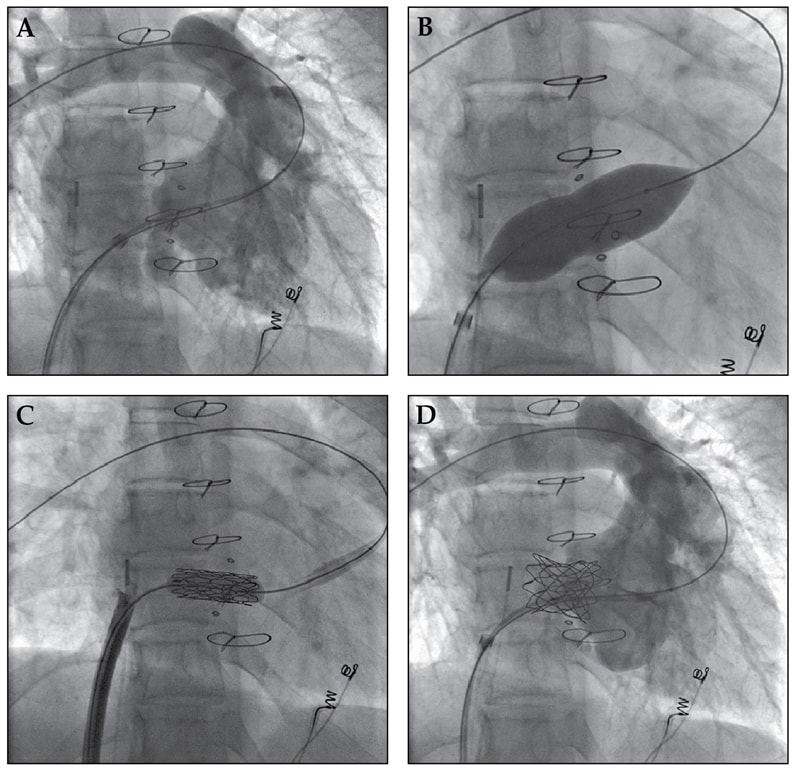
Tricuspid valve-in-valve implantation in a teenage patient with severe Ebstein anomaly and a 25-mm tissue bioprosthesis utilizes a Melody valve implanted on a 22-mm diameter delivery system. This patient has normal Melody valve function nearly four years after the procedure. A. Right ventricular angiogram demonstrates severe transvalvular regurgitation with brisk appearance of contrast in the right atrium. B. Static balloon sizing of the existing bioprosthesis is performed to determine implant valve type and size. C. Positioning of the Melody valve within the bioprosthesis from transfemoral approach with guidewire positioned in distal pulmonary artery branch. D. Right ventricular angiogram following successful valve implantation demonstrates complete resolution of tricuspid valve regurgitation.
Two types of transcatheter valves are being used in an off-label fashion, either a Melody (Medtronic Inc.) percutaneous valve or a Sapien (Edwards Lifesciences) valve. The type of valve used will depend on the size of the existing bioprosthesis (inner diameter) and nature of the valve dysfunction.
Allison Cabalka, M.D., a pediatric interventional cardiologist at Mayo Clinic in Rochester, Minnesota, and Charanjit S. Rihal, M.D., an interventional cardiologist and chair of Cardiovascular Diseases in the Center for Cardiovascular Sciences at Mayo Clinic in Rochester, Minnesota, are lead collaborators in a multicenter international registry. They have published results of transcatheter tricuspid valve implantation for treatment of dysfunctional surgical bioprosthetic valves in Circulation in 2016.
"Currently, over 40 patients have had tricuspid valve-in-valve implantation at Mayo Clinic with excellent results. Transvenous implantation is carried out via a femoral or an internal jugular approach; valve type and size are determined by the specifications of the existing bioprosthesis. Typically, the Melody valve is used for smaller diameter or tightly stenotic bioprosthetic valves, while the Sapien (S3, diameter up to 29 mm) is used for larger diameter bioprostheses," says Dr. Cabalka.
For the initial registry publication, data were collected on 156 patients with bioprosthetic TV dysfunction who underwent catheterization with planned tricuspid VIV. Patient median age in the registry cohort was 40 years with 71 percent of patients falling into NYHA class III or IV. After tricuspid VIV, both the tricuspid valve inflow gradient (stenosis) and degree of tricuspid regurgitation improved significantly.
The median post-catheterization hospital stay was two days. At follow-up, approximately 75 percent of patients were in New York Heart Association (NYHA) class I or II (p < 0.001 vs. pre-tricuspid VIV). Implant procedures were associated with a very low risk of complications, including paravalvular leak. Medium-term follow-up has been completed and longer term follow-up is in progress. Most patients continue to be treated with aspirin in addition to warfarin for anticoagulation to prevent valve thrombosis.
Mitral valve
Repeat operation in the first 10 years following mitral valve replacement is required in as many as 35 percent of patients. Repeat mitral valve replacement carries significant risk, making transcatheter treatment options appealing. Mitral VIV has been pioneered and performed successfully by Mayo Clinic physicians for over five years.
Transvenous transseptal mitral valve-in-valve procedure

Transvenous transseptal mitral valve-in-valve procedure
A. Balloon atrial septostomy is performed to allow Sapien valve (Edwards Lifesciences) delivery. B. Sapien valve is carefully positioned within the prosthesis over a left ventricular anchor wire. C. Balloon-expandable Sapien valve is deployed within the surgical valve. D. Equipment is removed.
"At Mayo Clinic, a total percutaneous approach is used via an antegrade transvenous transseptal delivery, in contrast to many centers where a predominantly transapical approach has been used. The total percutaneous approach allows for rapid patient recovery and relatively short hospital stays (median length of stay two days) in our most recent experience," says Mackram F. Eleid, M.D., an interventional cardiologist at Mayo Clinic in Rochester, Minnesota.
Results of a multicenter collaboration led by Mayo Clinic cardiologists and published in JACC Cardiovascular Interventions in 2016 has shown success rates greater than 90 percent with the transvenous transseptal mitral VIV procedure.
Similar to tricuspid VIV, the Sapien valve is most commonly used and size is selected based on the internal dimensions of the dysfunctional bioprosthesis and detailed perioperative imaging. Similar to tricuspid VIV, all patients are treated with aspirin and warfarin anticoagulation to prevent valve thrombosis. One-year follow-up data has been promising, but more long-term data is needed to understand the role of this exciting treatment option.
In summary, the goal with the structural heart team approach is to be able to provide comprehensive care to patients with complex valvular abnormalities (both congenital and acquired), with VIV therapy being an important part of comprehensive care in order to extend the life of surgically placed bioprosthetic valves.
For more information
McElhinney DB, et al. Transcatheter tricuspid valve-in-valve implantation for the treatment of dysfunctional surgical bioprosthetic valves. Circulation. 2016;133:1582.
Eleid MF, et al. Percutaneous transvenous transseptal transcatheter valve implantation in failed bioprosthetic mitral valves, ring annuloplasty, and severe mitral annular calcification. JACC Cardiovascular Interventions. 2016;9:1161.