Dec. 22, 2018
Mayo Clinic uses a novel technique for extensor mechanism reconstruction following total knee arthroplasty. The results for a large series of patients with midterm follow-up suggest that the stepwise surgical technique with Marlex mesh provides substantial functional benefit.
"We've had excellent results for an otherwise unsolved problem. At year four of mean follow-up, 84 percent of the mesh reconstructions were in place. Moreover, the mean extensor lag decreased from 36 to 10 degrees in our series," says Matthew P. Abdel, M.D., an orthopedic surgeon at Mayo Clinic in Rochester, Minnesota.
Disruption of the extensor mechanism after total knee arthroplasty is debilitating, and multiple methods of repair and reconstruction have had poor results. The key to Mayo Clinic's technique, described in the Aug. 1, 2018, edition of The Journal of Bone and Joint Surgery, is the stepwise approach, which helps ensure that the mesh is properly incorporated into the host soft tissues. The new technique builds on the reconstruction approach developed at Mayo Clinic by Arlen D. Hanssen, M.D., an emeritus consultant in Orthopedic Surgery.
"The procedure works well for people who have a complete disruption. However, we often see people referred for extensor mechanism disruptions who actually have a flexion contracture," Dr. Abdel says.
Ideally, patients should not have had previous surgery for extensor mechanism reconstruction. "In our series of 77 patients, about 1 in 4 had previous reconstruction attempts before referral to Mayo. While unfortunate, we are still able to salvage many of these limbs," Dr. Abdel says.
Complex surgery and rehabilitation
Mesh incorporated into host tissue distally
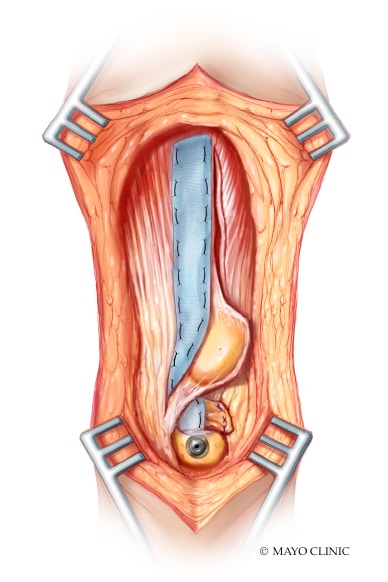
Mesh incorporated into host tissue distally
The mesh is incorporated into host tissue distally. The goal is for the mesh to pass through the host tissue via a tunnel, but to keep host tissue ventral and dorsal to the mesh to avoid any portion of the mesh rubbing on the prosthesis.
Mesh incorporated with the proximal tissue
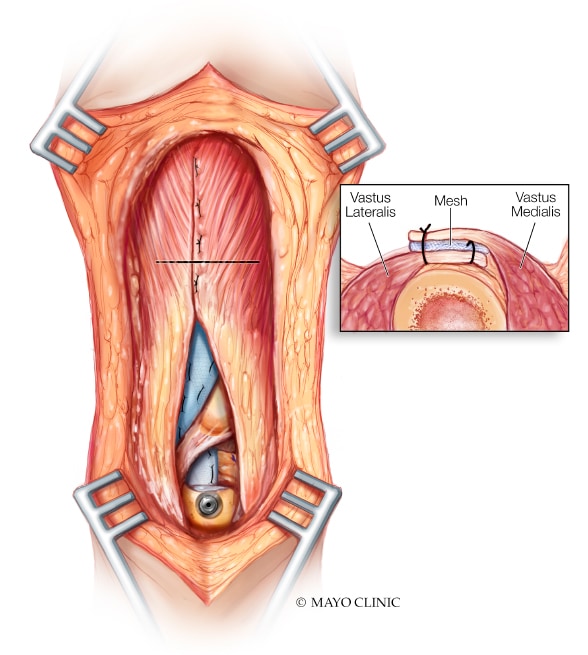
Mesh incorporated with the proximal tissue
The mesh is incorporated with the proximal tissue after aggressive ventral and dorsal mobilization of the vastus medialis obliquus and vastus lateralis.
The stepwise surgical technique entails:
- Securing the mesh to the tibia
- Ensuring that soft tissue completely covers the mesh so that it doesn't rub against the implant or beneath the skin
- Mobilizing the vastus lateralis and vastus medialis so that they cover the mesh
"Equally important to the success of this procedure is the postoperative rehabilitation. The casting is the second part of the surgery," Dr. Abdel says.
Patients have a full-length cast, which covers the foot, for three months. "The cast is changed every two to three weeks. We always change it here at Mayo Clinic, no matter where the patient is from," Dr. Abdel says.
After three months of casting, the patient wears a hinged knee brace and starts three to four months of physical therapy. The brace is locked in extension while the patient is ambulating and not doing therapy. Physical therapy can be done locally.
"The therapy protocol is quite involved and proceeds very slowly," Dr. Abdel says. "For the first month, we allow a maximum of 45 degrees of bend. In the second month, the maximum bend is 60 degrees; in the third, 75 degrees; and in the fourth, 90 degrees. For the next few months after that, patients can remove the brace, but I recommend that they use a walking aid so they don't have a buckling episode."
Future refinements of the technique might involve using a mesh with greater tensile strength, injecting stem cells to stimulate tissue growth of host tissues into the mesh and expanding the use of contemporary rotating-hinge prostheses to better stabilize the limb.
"Disruption of the extensor mechanism after total knee arthroplasty is rare, but the consequences for patients are catastrophic," Dr. Abdel says. "Mayo Clinic is committed to continually improving its techniques for the benefit of its patients."
For more information
Abdel MP, et al. Extensor mechanism reconstruction with use of Marlex mesh: A series study of 77 total knee arthroplasties. The Journal of Bone & Joint Surgery. 2018;100:1309.