May 17, 2025
Gynecologic Oncology at Mayo Clinic in Minnesota performs surgery to treat patients' cancers in circumstances under which other medical centers are unable to offer surgery.
"Patients with recurrent gynecologic cancer may have the opportunity to have a radical intervention with curative intent," says Amanika Kumar, M.D., a gynecologic oncologist at Mayo Clinic in Minnesota. "We may be able to assemble teams that can offer resection when other centers don't have those options."
She cites the circumstances of Becky, one of her patients who experienced a recurrence after ovarian and endometrial cancer treatment. A Mayo Clinic patient education video features Becky's story.
Standard care for patients with recurrent yet localized nonmetastatic gynecologic cancers is chemotherapy or radiation but usually not surgery. However, Dr. Kumar says Mayo Clinic gynecologic oncologists relish the challenge of treating patients with these uncommon surgical needs. They invite physicians to refer patients with complex gynecologic cancers, even if the disease appears surgically challenging.
When physicians refer patients with these cancers to Mayo Clinic in Minnesota, a multidisciplinary team including gynecologic surgeons, surgeons with other surgical specialties, psycho-oncologists and hyperbaric oxygen specialists supports the patient during the perioperative period. Dr. Kumar notes that Mayo Clinic has a high volume of supportive patient care services.
Pelvic exenteration and intraoperative radiation therapy
 Pelvic exenteration
Pelvic exenteration
Side and front views of a female pelvis. Organs shown in blue are removed in posterior pelvic exenteration surgery.
 Intraoperative radiation therapy
Intraoperative radiation therapy
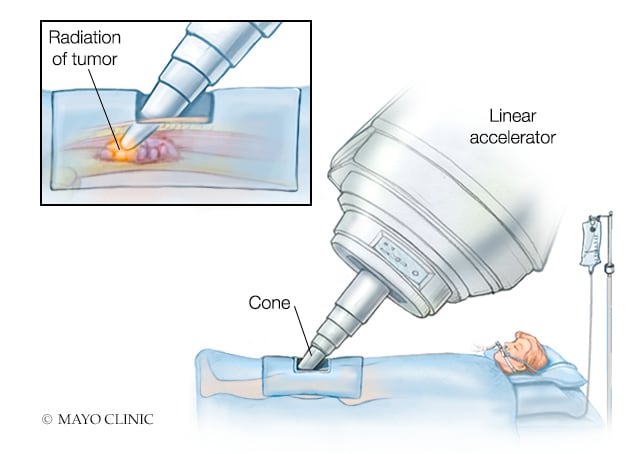
Intraoperative radiation therapy of tumor with a linear accelerator
Mayo Clinic offers patients with this type of gynecologic cancer recurrence lifesaving surgery through two procedures: pelvic exenteration (PE) and intraoperative radiation therapy (IORT). Community surgeons typically do not perform these procedures, and other academic medical centers may perform them infrequently, says Dr. Kumar.
PE
Dr. Kumar acknowledges that PE is considered radical surgery, yet she believes it offers hope for patients with otherwise poor prognoses. At Mayo Clinic, gynecologic oncologists offer PE to relieve severe pain, extend life, or cure recurrent or persistent pelvic cancers. PE eradicates recurrent disease by removing most pelvic organs: bladder, ovaries, uterus, vagina, rectum and lower colon. Gynecologic oncologists must balance the seemingly drastic nature of this surgery with patient benefits, including possible cure, she says.
PE complications
Because major complications can arise with PE, precise candidate selection is crucial, says Dr. Kumar. She and her colleagues undertook a study evaluating how physicians could anticipate patients' PE complications to help them make educated presurgical choices. The results were published in Gynecologic Oncology in 2019.
The study determined that 67% of patients undergoing PE experienced complications within 30 days; 27% experienced severe complications, such as organ system failure, infection, wound dehiscence and urinary reconstruction-related complications. Independent predictors of severe postsurgical complications included the extent of PE, presurgical hemoglobin less than or equal to 10 g/dL, and three or more comorbidities. These findings demonstrate the importance of patients' general health when considering PE, says Dr. Kumar.
"Complications are common, as are readmissions post-PE," she says. "Yet with the multidisciplinary care we have at Mayo Clinic, those complications are manageable."
PE's benefits and patient response to the surgery
The key benefit of PE is pain relief, says Dr. Kumar. For some patients, the benefit is even greater, she notes.
"At times, we can cure recurrent cancer with this procedure," she says. "This is unique, as recurrent cancer typically is challenging to cure."
Dr. Kumar and colleagues published an opinion statement on PE in Current Treatment Options in Oncology in 2023. They explained in this statement that with precise patient selection and a carefully composed team of specialists, including those in supportive care, PE can be a last curative option for some patients.
When a cure is possible, many patients are eager to proceed with this procedure despite its downsides, says Dr. Kumar. Her and her colleagues' roles are to operate on these patients and support them through challenging recoveries, she says.
"At the end of the day, with cancer treatment, there's a cost to everything we do," she says. "So helping patients understand options and treatments is imperative. We hope with this unique recurrent cancer care, we can offer patients improved survival and quality of life."
Need for expert counsel when considering PE
Physicians can counsel patients in weighing factors such as potential quality of life, surgical complications, and life expectancy with or without PE.
Despite the challenges PE presents, Dr. Kumar passionately believes it should be offered to appropriate patients.
Intraoperative radiation therapy (IORT)
Mayo Clinic in Minnesota's complex gynecologic oncology surgery is distinctive: Sometimes, along with PE, it offers IORT, a rare combination in this field, says Dr. Kumar.
IORT is especially useful for the treatment of advanced cancers in patients who might otherwise have no treatment options. Surgical staff move radiation equipment to the operating room and administer radiation directly to the exposed cancer site during surgery. Although many patients who have IORT also have presurgical standard radiation therapy, IORT can deliver a higher radiation dose to the cancer than that possible with standard radiation therapy.
Dr. Kumar and colleagues performed a study of IORT that included 80 patients with recurrent and persistent cervical or endometrial cancer, the results of which they published in a 2024 issue of Cancers. They found IORT safe and viable, given that surgeons thoughtfully selected patients for the procedure. The team also discovered that patients who had IORT experienced considerable survival benefit.
For more information
Tortorella L, et al. Prediction of short-term surgical complications in women undergoing pelvic exenteration for gynecological malignancies. Gynecologic Oncology. 2019;152:151.
Conway X, et al. RO resection in recurrent gynecologic malignancy: Pelvic exenteration and beyond. Current Treatment Options in Oncology. 2023:24; 262.
Howlett, LN, et al. Intraoperative radiation therapy for recurrent cervical and endometrial cancer: Predicting morbidity and mortality in a contemporary cohort. Cancers. 2024;16:3628.
Refer a patient to Mayo Clinic.