Feb. 15, 2018
All three Mayo Clinic campuses offer new, minimally invasive options for the diagnosis and treatment of medically refractory epilepsy. Stereoelectroencephalography (stereo EEG) and laser ablation of tissue are used to localize and treat seizure activity deep in the brain, allowing patients to avoid open surgery.
"Patients with medically refractory epilepsy can benefit hugely from surgery. But the invasive nature of a craniotomy to localize or treat seizures can make patients reluctant to take that step. Stereo EEG and laser ablation change that perception," says Richard S. Zimmerman, M.D., a neurosurgeon at Mayo Clinic in Phoenix/Scottsdale, Arizona.
For patients with medically refractory temporal lobe epilepsy, Mayo Clinic in Rochester, Minnesota, is enrolling participants in the Stereotactic Laser Ablation for Temporal Lobe Epilepsy (SLATE) clinical trial. Mayo Clinic's campus in Arizona will soon join the trial. SLATE is testing the efficacy of MRI-guided laser ablation for mesial temporal sclerosis that allows patients to avoid open temporal lobectomy.
"Rather than removing tissue so it will not cause seizures, we can heat the tissue, simply by inserting a laser catheter. Through advanced imaging we can see in real time exactly what tissue we're treating, so we are very accurate," says Jamie J. Van Gompel, M.D., a neurosurgeon at Mayo Clinic in Rochester, Minnesota, and the trial's principal investigator at that site. Successful application of these sophisticated techniques requires close collaboration between neurologists and neurosurgeons. At Mayo Clinic, neurological and neurosurgical services are completely integrated.
"Stereo EEG and laser ablation are truly expressions of what we can do when neurology and neurosurgery work together as a neuroscience team," says William Tatum, D.O., a neurologist at Mayo Clinic in Jacksonville, Florida. "These procedures can give patients a second look at life. Without it they are neurologically disabled — they often can't drive, can't make a living, can't form interpersonal relationships and have a poor quality of life."
Stereo EEG
Positioning of electrodes for stereoelectroencephalography
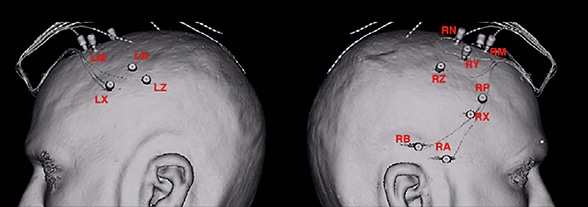
Positioning of electrodes for stereoelectroencephalography
Illustrations indicate the positioning of electrodes for stereoelectroencephalography. On the left, positioning is indicated in the left anterior supplementary motor area (LM), left posterior supplementary motor area (LN), left anterior cingulate (LX) and left posterior cingulate (LZ). On the right, positioning is indicated in the right anterior temporal lobe (RA), right posterior temporal lobe (RB), right anterior supplementary motor area (RM), right posterior supplementary motor area (RN), right far anterior cingulate (RP), right anterior cingulate (RX), right middle cingulate (RY) and right posterior cingulate (RZ).
Electrodes placed deep in the brain
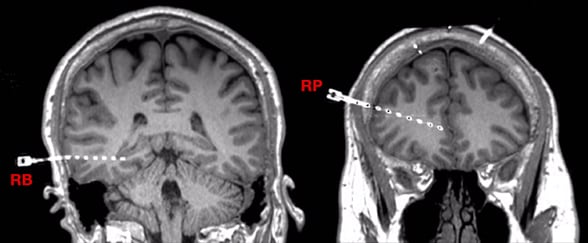
Electrodes placed deep in the brain
Imaging shows the placement of electrodes in the right posterior temporal lobe (RB) and right far anterior cingulate (RP).
Stereo EEG involves drilling several very small access holes measuring about 2.3 millimeters in diameter in the skull. Under computer-guided navigation, electrodes can then be placed deep in the brain to map seizure activity and nearby important and functional tissue.
"Stereo EEG allows us to record from areas in the brain that previously were very difficult to access with electrodes," says Amy Z. Crepeau, M.D., a neurologist at Mayo Clinic's campus in Arizona. "When noninvasive testing isn't enough to zero in on the seizure onset zone, stereo EEG allows us to record from a wider area in the brain. Patients tolerate this method much better than craniotomy and recover more quickly."
The electrodes are placed under general anesthesia. Patients sometimes spend several days in the epilepsy monitoring unit before returning to the operating room for removal of the electrodes. The neurosurgeon might remove the seizure onset zone at that time or wait a few weeks if the patient needs additional time to recover from the monitoring.
"With stereo EEG, we're seeing epilepsies in all sorts of locations — the insular cortex, the cingulate cortex — that we never saw before," Dr. Van Gompel says. "Stereo EEG is system mapping that can probe various areas of the brain that communicate with one another even though they're not adjacent."
Once seizure activity is localized, laser ablation can sometimes be used to treat epileptic tissue. "We're able to combine the minimally invasive diagnostic procedure with a minimally invasive therapeutic approach, sometimes in the same hospitalization," Dr. Zimmerman says. "Obviously, that depends on the amount of tissue that's causing the seizures and its location. If it's a large area of the brain, the patient may need an open surgery. If the site is in an eloquent area, we might implant a neurostimulation device."
Enrolling patients in SLATE
SLATE is a phase 1, multicenter clinical trial. The MRI-guided system has approval from the Food and Drug Administration for ablation of brain tissue but isn't indicated for epilepsy treatment. In the trial, about 150 adults between the ages of 18 and 70 will have MRI-guided laser ablation of the amygdala and hippocampus. Over 12 months, study participants will be evaluated for freedom from seizures, quality of life, adverse events and neuropsychological outcomes.
"The big advantage is patient recovery," Dr. Van Gompel says. "With laser ablation, the patient generally stays in the hospital just overnight and can return to normal activities in a week or so. Open temporal lobectomy means a three-day hospitalization and six to 12 weeks for recovery. "We tell our patients that we have a higher chance of curing them with the open surgery, but the less invasive laser procedure has a good chance of working," he adds. "If it doesn't, we can still do the open procedure that carries an increased risk."
QT grid for localizing seizures
In addition to stereo EEG, neurologists and neurosurgeons at Mayo Clinic's Florida campus use a unique intraoperative brain mapping tool, often with the patient awake. The device, known as a QT grid, is a 4-centimeter ring with 22 sensors around the perimeter. It was developed by Dr. Tatum and Alfredo Quinones-Hinojosa, M.D., chair of Neurosurgery at Mayo Clinic's Florida campus.
The circular grid can surround small areas of the brain, to precisely identify seizure location. Keeping patients awake allows for dynamic testing during the procedure to avoid damage to eloquent tissue.
"We have had extraordinarily positive results in our ability to resect parts of the brain that appear to be misfiring. In many cases we have had resolution of the epilepsy," Dr. Quinones-Hinojosa says. "We are combining our extensive experience with awake brain surgery and our neurological expertise with seizures.
"Mayo Clinic is truly the world-class leader for integrated multispecialty practice," he adds. "The culture of excellence is so tightly woven that we work as a true unit, both inside and outside the operating room, to ensure that the needs of the patient come first."
For more information
Medtronic Navigation Inc. Stereotactic Laser Ablation for Temporal Lobe Epilepsy (SLATE). ClinicalTrials.gov.