May 30, 2025
Mayo Clinic takes a proactive approach to caring for people with a family history of intracranial aneurysm. A multidisciplinary team works to screen at-risk individuals and determine the best options to prevent life-threatening brain bleeds.
"The risk of rupture is 15-20 times higher in people with familial aneurysms compared with sporadic aneurysms," says Bernard R. Bendok, M.D., chair of Neurosurgery at Mayo Clinic in Phoenix/Scottsdale, Arizona. "Familial aneurysms also tend to rupture about a decade earlier. Anyone who has two family members with an intracranial brain aneurysm should get screened."
That recommendation echoes guidance from the American Heart Association and the American Stroke Association. "Unfortunately, we regularly see individuals with a ruptured intracranial aneurysm who had knowledge of a family history of the condition but were never screened," says Bart M. Demaerschalk, M.D., a neurologist at Mayo Clinic. "We always see that as a missed opportunity."
Screening is particularly important for people with additional risk factors. "Smoking triples or quadruples the risk of rupture. For smokers with hypertension, the risk of rupture may go up 10-fold," Dr. Bendok says.
Mayo Clinic neurologists and neurosurgeons have deep experience managing challenging cerebrovascular malformations. As a tertiary center, Mayo Clinic also has geneticists and experts in managing conditions associated with familial vascular malformations, such as connective tissue disorders and autosomal dominant polycystic kidney disease (ADPKD).
"We can't screen everyone," Dr. Bendok says. "But we need to work toward strategic screening."
Seamless, personalized care
Mayo Clinic strives to optimize the patient care experience. Initial telehealth consultations are offered to patients before they arrive on the Arizona campus. During telehealth visits a neurologist or neurosurgeon or both can review external health records and imaging and take a short patient history.
"The purpose of these consultations isn't to make a diagnosis or render care but to make the patient's on-site care more efficient," Dr. Demaerschalk says. "We can determine what incremental diagnostic studies might be needed and which specialists the patient needs to see. Our patients tell us that they favor that early contact because it makes their arrival on campus more comfortable. It eases their minds."
 Excellent spatial resolution
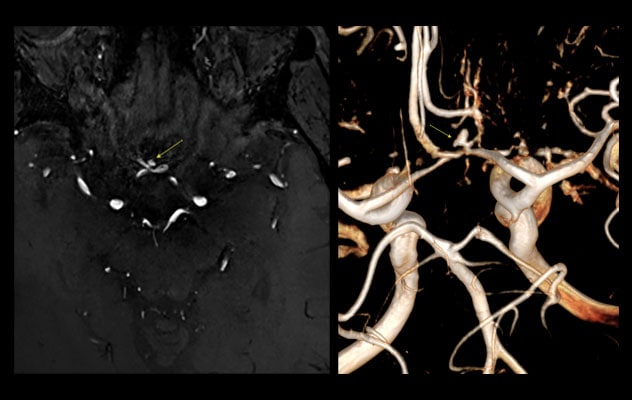
Excellent spatial resolution
7T MRAs show a 3 millimeter right A1/A2 junction aneurysm (arrows) in a 68-year-old man.
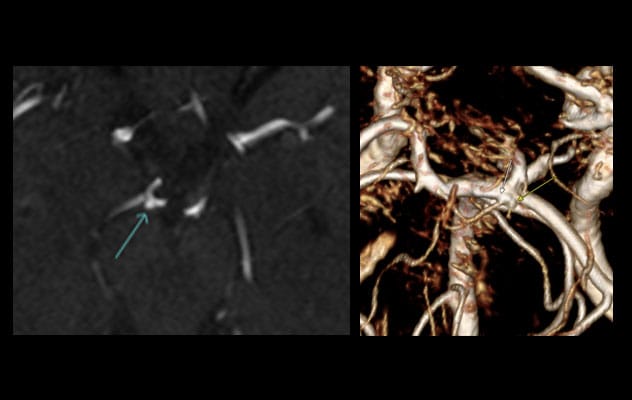 Distinguishing aneurysm from infundibula
Distinguishing aneurysm from infundibula
On the left, 3T MR angiogram (MRA) shows a possible aneurysm (arrow) in the right P1/P2 junction in a 55-year-old woman. On the right, 3D maximum intensity projection of a follow-up 7T MRA shows two separate and distinct vessels in that region with conical outpouchings (arrows) consistent with infundibula.
Once patients are on campus, imaging is interpreted by subspecialized neuroradiologists. "The biggest challenge in screening for aneurysms is false positives," says Nick G. Matthees, M.D., a neuroradiologist at Mayo Clinic's campus in Arizona. "We are fortunate to have both photo-counting-detector CT angiogram and 7T MRI, both of which have excellent spatial resolution. That allows us to better distinguish aneurysms from infundibula."
A multidisciplinary team develops a treatment plan. Endovascular coiling, flow diversion or a surgical clip typically is used. Open surgery or radiotherapy might occasionally be recommended.
Virtual 3D models of aneurysms are used to rehearse aneurysm surgeries. The models also can be superimposed over a patient's anatomy for intraoperative guidance. "We have a unique augmented reality surgical platform," Dr. Bendok says. "We're also able to seamlessly integrate open surgery and endovascular therapy."
"We need to work toward strategic screening."
Like familial aneurysms, hereditary arteriovenous malformations (AVMs) pose distinct challenges. Mayo Clinic specialists have experience with the diagnosis and treatment of hereditary hemorrhagic telangiectasia (HHT), a disorder that causes AVMs in multiple organs.
"Those AVMs can cause bleeding from the nose, lungs, brain and elsewhere. They are often small and can be difficult to diagnose," Dr. Bendok says. "HHT requires care at a center that specializes in the imaging and management of these rare AVMs." Mayo Clinic's multidisciplinary HHT team includes specialists in radiology, pulmonology, otolaryngology (ENT) and genetics.
Mayo Clinic's physician-scientists are working to better understand risks associated with familial cerebrovascular malformations. The results of a study published in the Journal of Neurosurgery suggest that ADPKD patients who are female, have a family history of intracranial aneurysm or subarachnoid hemorrhage, or have moderate or more severe PKD would benefit from early screening for intracranial aneurysm even if neurologically asymptomatic.
Led by Dr. Bendok, Mayo Clinic's Neurosurgery Simulations and Innovations Laboratory is working to develop a risk calculator to predict which patients will experience intracranial aneurysm rupture.
"We don't want to wait for aneurysms to rupture," Dr. Bendok says. "Most healthcare since Hippocrates has been reactive. The future of healthcare needs to be proactive."
For more information
Nguyen BA, et al. Risk factors for unruptured intracranial aneurysms in asymptomatic patients with autosomal dominant polycystic kidney disease: Who needs screening? A systematic review and meta-analysis. Journal of Neurosurgery. In press.
Neurosurgery Simulation and Innovations: Bernard R. Bendok. Mayo Clinic.
Refer a patient to Mayo Clinic.