Sept. 14, 2018
A 43-year-old man presented for evaluation of an incidentally discovered pituitary mass. His past medical history was notable for alveolar soft part sarcoma of the thigh resected 19 years previously. After a disease-free period of 16 years, the patient developed bilateral lung metastases, which were treated surgically. One year ago, he developed a metastasis in the pancreatic tail, which was resected, and another metastasis in the left kidney, treated with radiofrequency ablation. As a part of cancer surveillance, a brain MRI was obtained and it showed right-sided pituitary enlargement with mild extension into the suprasellar cistern and deviation of the infundibulum to the left. The patient had no symptoms suggestive of pituitary dysfunction except for minimal fatigue. He did not have headaches or visual symptoms.
Hormonal evaluation at initial presentation
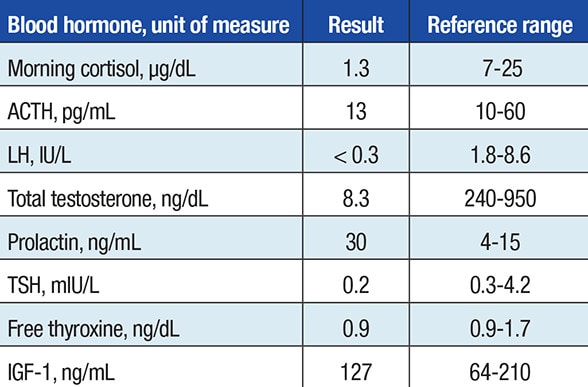
Hormonal evaluation at initial presentation
Hormonal evaluation at initial presentation with a pituitary mass. Laboratory testing demonstrated secondary adrenal insufficiency and hypogonadotropic hypogonadism.
Despite his asymptomatic state, laboratory testing demonstrated secondary adrenal insufficiency and hypogonadotropic hypogonadism. Visual field testing was normal. The patient was initiated on glucocorticoid and testosterone replacements.
Head MRI shows a 21-by-16-millimeter sellar mass
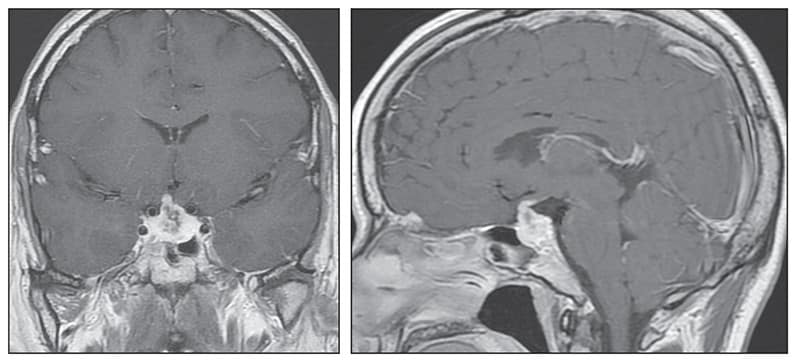
Head MRI shows a 21-by-16-millimeter sellar mass
Head MRI (coronal image on left and sagittal image on right) shows a 21-by-16-millimeter sellar mass causing superior displacement of the optic chiasm and thickening of the pituitary stalk — new findings when compared with a head CT obtained two years previously.
Hypopituitarism is very uncommon with primary pituitary tumors and in view of his history of metastatic alveolar soft part sarcoma, a pituitary metastasis was suspected. Complete surgical resection of the pituitary mass was not considered feasible, and the tumor was treated with Gamma Knife radiosurgery. Six months after radiosurgery, the pituitary-directed head MRI showed heterogeneous hypoenhancement of the central pituitary gland consistent with post-radiation changes.
Metastases to the pituitary gland are rare and usually present with symptoms of pituitary dysfunction, visual disturbances, cranial nerve deficits or headaches, as documented in studies published in the Journal of Neuro-Oncology in 2016 and The Endocrinologist in 2002. In a Mayo Clinic series of 52 patients with intrasellar metastases diagnosed between 1950 and 1996, there were 29 women and 23 men with a mean age of 60 years. Findings include the following:
- Breast and lung carcinomas were the most frequent primary tumors (37 percent and 23 percent, respectively).
- The primary tumor was unknown in 12 percent of patients.
- In the patients with a known primary tumor, it was diagnosed after the pituitary metastasis was discovered in 20 percent.
- The mode of discovery of pituitary metastases was symptom based (visual impairment, diabetes insipidus, hypopituitarism) in 75 percent of patients.
- Of the patients in whom prolactin was measured, 63 percent had hyperprolactinemia.
- Pituitary surgery and radiotherapy were performed in 42 percent and 63 percent of patients, respectively.
- Mean survival was 17 months (range, 0-240 months). Overall mortality at one year was 67 percent.
Histologic confirmation of metastatic disease is usually performed; however, when the imaging characteristics are suggestive of metastasis in a patient with a known metastatic disease at other sites, biopsy is not necessary, especially if it will not change subsequent management.
Little evidence exists in regard to the best treatment approach for pituitary metastases. Because of the poor prognosis associated with sellar metastases, the most reasonable therapeutic approaches are palliative radiotherapy, pituitary target hormone replacement therapy when indicated and primary tumor-directed chemotherapy. Surgical debulking of the sellar metastasis may be beneficial in patients with visual field defects caused by compression of the optic chiasm.
Total resection of the pituitary tumor can be difficult because of invasion of surrounding structures and increased vascularity. Recovery of pituitary function is unlikely to occur after surgery, but visual symptoms may improve. Radiosurgery also can be performed after initial surgical debulking in an attempt to stop local tumor regrowth.
Management of patients with pituitary metastasis should be individualized after consideration of presenting symptoms, imaging characteristics, goals of treatment and patient's preferences.
For more information
Gilard V, et al. Pituitary metastasis: Is there still a place for neurosurgical treatment? Journal of Neuro-Oncology. 2016;126:219.
Heshmati HM, et al. Metastases to the pituitary gland. The Endocrinologist. 2002;12:45.