Sept. 10, 2014
Most patients with papillary thyroid cancer (PTC) present with disease confined to the thyroid; however, neck nodal metastases (NNM) may be found in up to 40 percent of patients at the time of initial surgical resection. Despite potentially curative primary operative intervention, approximately 15 percent of patients with PTC are also later found to have NNM — discovered months to years after the initial operation. Recent advances in neck ultrasound and thyroglobulin-directed detection of small NNM presents the endocrinologist with a dilemma in terms of best management.
Ian D. Hay, M.D., Ph.D., of the Division of Endocrinology, Diabetes, Metabolism, and Nutrition at Mayo Clinic's campus in Rochester, Minnesota, says: "It is being increasingly recognized that radioiodine remnant ablation rarely prevents the later discovery of postoperative NNM in PTC. Reoperative, compartment-oriented surgery, recommended by most management guidelines for the treatment of recurrent NNM, unfortunately produces a biochemical remission in only 30 to 50 percent of cases.
"Our group first used ultrasound-guided percutaneous ethanol ablation (UPEA) in the management of recurrent NNM in PTC in 1993, and in 2002 we reported that it was a safe, effective and considerably less expensive alternative to operative management. In 2013, we reported on the long-term efficacy of UPEA in the initial control of 37 recurrent NNM in 25 patients with advanced localized disease (pTNM stages III or IVA) who had previously been treated by both primary definitive surgery and postoperative RAI therapy."
Of the 25 ablated patients:
- 10 (40 percent) had only central nodes ablated
- One had both central and lateral nodes treated
- 14 (56 percent) had lateral nodes only
Patient with recurrent metastatic papillary thyroid cancer in a hypervascular right neck lymph node

Patient with recurrent metastatic papillary thyroid cancer in a hypervascular right neck lymph node
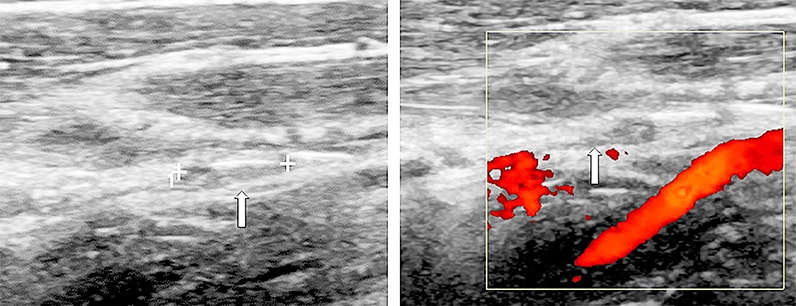
Neck ultrasound images with Doppler flow image on right show recurrent metastatic papillary thyroid cancer in a hypervascular right neck lymph node (arrows) with a calculated lymph node volume of 168 mm3 prior to ethanol ablation.
Patient with recurrent metastatic papillary thyroid cancer 10 months after ultrasound-guided percutaneous ethanol ablation
Patient with recurrent metastatic papillary thyroid cancer 10 months after ultrasound-guided percutaneous ethanol ablation
Neck ultrasound images, with Doppler flow image on right. Ten months after ultrasound-guided percutaneous ethanol ablation, the patient's treated lymph node (arrow) is now small and hypovascular with a calculated lymph node volume of 12 mm3.
Robert A. Lee, M.D., of the Department of Radiology at Mayo Clinic in Rochester, Minnesota, explains: "The largest diameter of treated nodes ranged from 4 to 21 mm (mean, 14). UPEA was typically performed in two sessions on consecutive days. Seven of 25 patients (28 percent) had further sessions (average one more), typically three to six months later, to completely eliminate Doppler flow in the NNM. The volume of ethanol injected per session ranged from 0.1 to 1.4 mL, and the average injection was 0.5 mL."
Efficacy of UPEA
Dr. Hay highlights: "In this series of 37 NNM treated by UPEA, tumor perfusion, as evidenced by Doppler blood flow, was eliminated in each ablated node after successful therapy. After a mean follow-up of 65 months (range, 5 to 157), 17 ablated NNM (46 percent) completely disappeared on ultrasound rescanning. During follow-up, six of the 25 patients (24 percent) developed 18 new NNM; 15 of the 18 (83 percent) were managed successfully by UPEA, rather than by neck re-exploration.
"Serum thyroglobulin (Tg) levels were meaningfully followed in the 22 patients without Tg autoantibodies. Optimal Tg values of < 0.2 ng/mL on thyroid hormone suppressive therapy (THST) were found at last follow-up in 12 of the 22 (55 percent).
"Intermediate Tg levels of 0.3 to 2.4 ng/mL were seen in six (27 percent) without demonstrable disease; and unacceptable serum Tg values of > 2.5 ng/mL were seen in four (18 percent) who had persistent PTC in NNM, which was biopsy proven in all four cases."
Complications
Dr. Lee notes: "Most patients experienced brief discomfort at the UPEA site. In all of these patients, the discomfort resolved after several minutes. None of the 25 patients undergoing UPEA of the initial 37 NNM experienced, as a consequence of their UPEA, transient or permanent hoarseness or vocal cord paralysis."
Treatment goals
Treatment goals, in order of importance, include:
- Elimination of significant nodal blood flow ("tumor perfusion") by Doppler ultrasonography
- Reduction in volume of treated NNM, ideally to the point of disappearance on rescanning
- When possible, concomitant reduction in circulating serum Tg levels on THST
"In our 2013 report, 46 percent of the ablated NNM disappeared on rescanning and 35 of 37 of the treated nodes (95 percent) had decreased tumor volumes after successful UPEA. We considered post-UPEA serum Tg levels of < 0.2 ng/mL as optimal and levels of < 2.5 ng/mL as acceptable in the context of advanced localized disease," says Dr. Hay.
The average charge for each of 75 UPEA procedures performed during 2010 at Mayo Clinic for 53 PTC patients was $1,583, a fraction of the $35,000 to $45,000 in charges estimated (including all hospitalization costs) for either a central compartment node dissection or a unilateral modified radical neck dissection.
Conclusion
Dr. Hay concludes: "It is our opinion that UPEA should be more generally incorporated into the management of NNM in advanced localized PTC not amenable to conventional retreatment with surgery, radioiodine or external irradiation. Moreover, our 25 patients, by avoiding 40 further neck explorations, on average saved themselves at least $61,000 in medical charges."