Oct. 20, 2022
Ventricular arrhythmia is a rare occurrence in the pediatric population and is often an unexpected finding in patients with otherwise normal hearts. However, when a child does present with ventricular arrhythmia, specific causes warrant consideration and guide the subsequent work-up and treatment strategy.
Patients with known heart disease — for example, congenital heart disease, cardiomyopathy or channelopathies — may be at risk of ventricular arrhythmia and require a different approach compared with patients who have normal hearts. Ventricular arrhythmia in a normal heart can range from infrequent ectopy to incessant ventricular tachycardia (VT).
Premature ventricular complexes
Premature ventricular complexes (PVCs) are a common finding in pediatric patients of all ages and may be seen on a Holter monitor in about 40% of otherwise healthy children. When PVCs are rare, isolated and monomorphic, they usually do not require extensive evaluation in an otherwise healthy child and have an excellent prognosis. Spontaneous resolution over time is quite possible and is more likely the younger the patient is at the time of presentation.
However, when the PVC burden is more frequent or more complex — that is, multiform PVCs, couplets or nonsustained VT — it necessitates further work-up and possibly longitudinal follow-up.
Pediatric ventricular arrhythmia evaluation
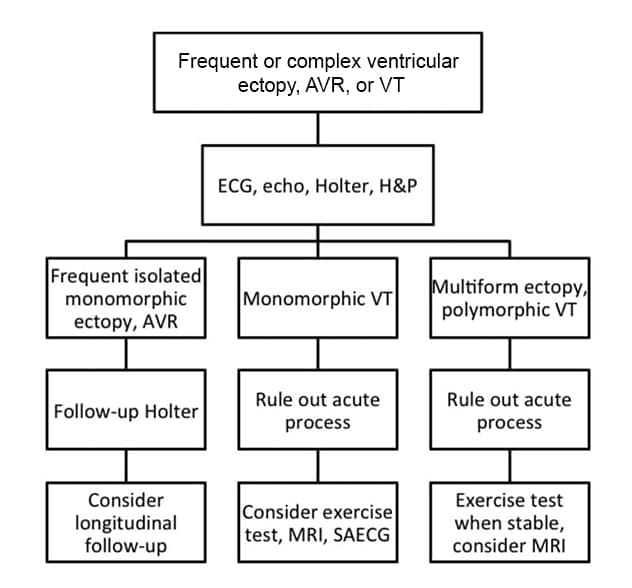
Pediatric ventricular arrhythmia evaluation
AVR, accelerated ventricular rhythm; ECG, electrocardiogram; echo, echocardiogram; H&P, history and physical examination; MRI, magnetic resonance imaging; SAECG, signal-averaged electrocardiogram; VT, ventricular tachycardia
The initial work-up for frequent or complex PVCs should include electrocardiography, echocardiography, Holter monitoring, and thorough history taking and physical examination to assess for underlying heart disease such as myocarditis, cardiomyopathy and channelopathies.
With frequent ectopy (generally defined as 10% of beats or more in a 24-hour period), there is a risk of developing ventricular dysfunction even in a normal heart. The exact PVC burden at which ventricular dysfunction may occur is unclear, but in most studies, 20% to 30% ectopy is needed to increase the risk of ventricular dysfunction.
"Treatment of PVCs in the setting of a normal heart is rarely required," according to Philip L. Wackel, M.D., a pediatric cardiologist at Mayo Clinic Children's Center in Rochester, Minnesota. "Declining ventricular function or symptomatic complaints of palpitations that are clearly attributable to the PVCs are two situations in which treatment may be warranted."
The usual first line treatment is medical therapy, and often a β-blocker is used; however, calcium channel blockers also could be considered as first line agents in patients older than 1 year.
If these medications fail or have adverse effects, a number of second line anti-arrhythmics could be started or catheter ablation could be attempted. Catheter ablation is generally highly successful in eliminating a single PVC focus. However, the risks of the procedure must be weighed carefully against the indication and the chance for spontaneous resolution with time.
Accelerated ventricular rhythm
It is important to differentiate accelerated ventricular rhythm (AVR) from VT in pediatric patients because the prognosis differs. The exact rate at which this distinction is made varies with age and is based on the rate of the ventricular arrhythmia compared with sinus rhythm.
AVR is generally defined as rates up to 15% to 20% faster than the expected sinus rate or up to 120 beats a minute in an older teenager at rest. AVR is typically benign, rarely requires treatment and carries the same excellent prognosis as PVCs. AVR can occur at any age and may present as early as the first hours of life.
"In the absence of heart disease, metabolic derangements or electrolyte abnormalities, AVR in the neonate is usually also benign but does require longitudinal follow-up until the arrhythmia resolves to ensure ventricular function remains normal," says Dr. Wackel.
Neonatal AVR usually resolves within the first year of life. AVR presenting in older children can be followed as isolated PVCs are, as discussed previously, with longitudinal follow-up to assess the burden of ectopy and for the potential development of ventricular dysfunction if the ectopy is frequent.
Monomorphic VT
There are several distinct clinical scenarios in which a child with a normal heart can have VT, and these carry a much different prognosis than VT in an abnormal heart. Therefore, establishing that a heart is normal is vital before entertaining one of the common causes of normal-heart VT in a child. The initial evaluation should thus be aimed at confirming that a heart is indeed normal and that there are no acute causes of VT.
The appearance of some types of benign VT can overlap with that of arrhythmogenic right ventricular cardiomyopathy, myocarditis, cardiomyopathy or channelopathies. Therefore, ruling out underlying heart disease in the face of VT also may require additional testing with an exercise stress test, cardiac MRI, signal-averaged electrocardiogram or all three. Once a heart is determined to be completely normal, the causes of VT are generally benign.
The most common cause of childhood VT in a normal heart is right ventricular outflow tract (RVOT) tachycardia. This accounts for 60% to 80% of all childhood VT in a normal heart. Typically, childhood VT is caused by a single focus in the RVOT and results in a single QRS morphology with an inferior axis and left bundle branch block morphology.
Less commonly, the focus can originate from areas outside but near the RVOT, such as from above the pulmonary valve, from near the bundle of His, and from the left ventricular outflow tract or aortic cusps. Careful evaluation of the QRS morphology often can help more specifically localize the focus.
The mean age of presentation is 8 years, and childhood VT may be discovered incidentally. Many patients with RVOT tachycardia will be asymptomatic, but symptoms of palpitations or near syncope also are commonly seen. However, true syncope is uncommon and warrants further investigation for an alternative diagnosis.
Additional work-up beyond the basic testing may include an exercise stress test because typically, RVOT tachycardia suppresses with exercise, although there is a variant that increases with exercise. Despite the response to exercise, RVOT tachycardia should remain monomorphic, and polymorphic ectopy seen with exercise strongly suggests an alternative diagnosis.
The prognosis of RVOT tachycardia is usually benign, and many patients eventually have spontaneous resolution or a declining ectopy burden over time when the condition persists. Similar to the management of PVCs and AVR, treatment is recommended only if symptoms are bothersome or if ventricular dysfunction occurs. If treatment is indicated, as in PVCs, usually β-blockers, calcium channel blockers or both are used as the first line treatment, with second line anti-arrhythmics and ablation as alternatives.
Another common cause of monomorphic VT is posterior fascicular VT, also referred to as verapamil-sensitive VT or Belhassen VT. This VT accounts for 10% 15% of childhood VT in a normal heart. This tachycardia is due to a reentrant circuit typically involving the left posterior fascicle, but it can involve any portion of the fascicle.
Electrocardiogram of posterior fascicular ventricular tachycardia
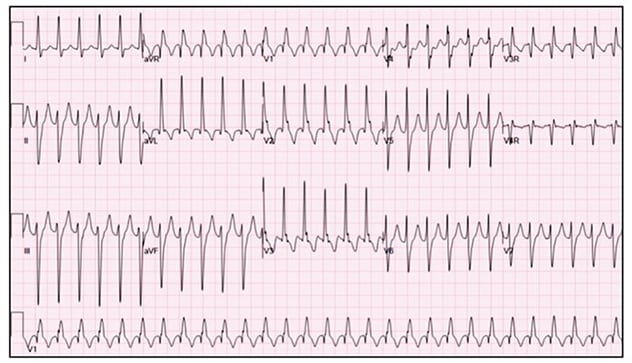
Electrocardiogram of posterior fascicular ventricular tachycardia
A common cause of monomorphic VT is posterior fascicular VT, which is due to a reentrant circuit typically involving the left posterior fascicle. Typically, this circuit results in a QRS morphology that is relatively narrow compared with that of other types of VT, and it usually has a superior axis with right bundle branch morphology.
Typically, this circuit results in a QRS morphology that is relatively narrow compared with that of other types of VT, and it usually has a superior axis with right bundle branch morphology. This type of VT commonly occurs as sustained episodes of monomorphic VT and may be brought out with exercise. It is generally well tolerated at slower rates less than 200 beats a minute. As the name implies, it is highly responsive to intravenous verapamil in the acute setting and may be treated with oral verapamil moving forward to attempt to prevent future recurrence.
However, 20% of patients experience breakthrough episodes of VT despite treatment with oral verapamil. In such cases, alternative anti-arrhythmics or ablation may be considered. Ablation can be safely accomplished in pediatric patients who weigh more than 15 kilograms, but varying degrees of success have been reported. In the largest study of fascicular VT ablation in pediatric patients, the initial success rate was 72%, with a recurrence rate of 18%. Therefore, a common approach to management of fascicular VT has been to treat it medically until the child is larger, at which time ablation can be attempted.
A rare form of incessant VT seen in the newborn period is usually monomorphic and arises most commonly from the left ventricle. Monomorphic VT of the newborn has been associated with ventricular tumors. Commonly it is an isolated hamartoma (Purkinje cell tumor), although in 50% of cases no etiology is identified. Neonatal myocarditis also should be ruled out. The VT rate may be very fast and is often higher than 200 beats a minute.
The QRS duration in neonatal VT can be relatively narrow and may be as short as 60 milliseconds, which can sometimes make differentiating incessant VT from supraventricular tachycardia difficult. Careful comparison of the QRS in tachycardia to the QRS in sinus rhythm can help make this distinction. Incessant VT of the newborn may be associated with tachycardia-induced cardiomyopathy, especially in patients in whom more than 80% of the day is spent in VT.
Anti-arrhythmic medication is almost always required to achieve a level of control to avoid tachycardia-induced cardiomyopathy and maintain adequate perfusion. Most infants with incessant VT have spontaneous resolution in 1 to 2 years, at which point they can be weaned from anti-arrhythmics. However, mortality in this disorder may be as high as 15% related to tachycardia-induced cardiomyopathy.
Polymorphic VT
Polymorphic VT defined as beat-to-beat variations in the QRS morphology, QRS axis or both during VT is rare in childhood and generally carries a worse prognosis than monomorphic VT. It is even more uncommon for children to have polymorphic VT with no underlying heart disease, as it is almost always associated with an underlying cardiac abnormality.
Therefore, the presence of multiform ventricular ectopy or polymorphic VT in a child warrants a thorough investigation into underlying structural heart disease, cardiomyopathy, myocarditis and channelopathies. In addition, metabolic or electrolyte abnormalities, medication toxicity, illicit drug use, and in the case of neonates, toxicity from the mother's use of medications or recreational drugs should be investigated.
"Even if no etiology is identified, these patients warrant longitudinal follow-up and, depending on the degree of ectopy and symptoms, may require anti-arrhythmics or even implantation of an internal cardioverter-defibrillator, depending on the severity of the presentation," says Dr. Wackel.
For more information
Refer a patient to Mayo Clinic.