Diagnosis
To diagnose peripheral nerve injuries, your healthcare professional reviews your medical history. You're asked about any accidents or previous surgeries you've had and about your symptoms. Your healthcare professional also conducts a physical and neurological exam. If there are symptoms of a nerve injury, you may need diagnostic tests, which may include:
- Electromyography (EMG). In an EMG, a thin-needle electrode inserted into the muscle records the muscle's electrical activity at rest and in motion. Reduced muscle activity can suggest nerve injury.
- Nerve conduction study. Electrodes placed at two different points in the body measure how well electrical signals pass through the nerves.
- Magnetic resonance imaging (MRI). MRI uses a magnetic field and radio waves to produce detailed images of areas affected by nerve damage.
- Ultrasound. Like MRI, these high-frequency sound waves produce detailed images of the area affected by nerve damage.
Treatment
If a nerve is injured but not cut, the injury is more likely to heal. Injuries in which a nerve has been completely cut are harder to treat, and recovery may not be possible.
Your treatment is based on the extent and cause of your injury and how well the nerve is healing.
- If your nerve is healing properly, you may not need surgery. You may need to rest the affected area until it's healed. Nerves recover slowly, and maximal recovery may take many months or several years.
- Regular checkups allow your healthcare professional to make sure your recovery is on track.
- If your injury is caused by a medical condition, your healthcare professional treats the condition.
- Depending on the type and severity of your nerve injury, you may need medicines such as aspirin or ibuprofen (Advil, Motrin IB, others) to relieve your pain. Medicines used to treat depression, seizure or insomnia may be used to relieve nerve pain. Some people with peripheral nerve injuries may need corticosteroid injections for pain relief.
- Your healthcare professional may recommend physical therapy to prevent stiffness and restore function.
Surgery
If your injury does not seem to be healing properly, you may need surgery. A surgeon can use EMG testing in the operating room to assess whether scarred nerves are recovering. Doing an EMG test directly on the nerve is more accurate and reliable than doing the test over the skin.
Sometimes a nerve sits inside a tight space similar to a tunnel or is squeezed by scarring. When this happens, a surgeon may enlarge the tight space or free the nerve from the scar.
If a section of an injured nerve is cut completely or damaged beyond repair. A surgeon can remove the damaged section and directly reconnect healthy nerve ends. This is known as nerve repair. Or the surgeon may implant a piece of nerve from another part of the body to close a gap between the nerves. This is known as a nerve graft. These procedures can help nerves regrow.
Peripheral nerve graft
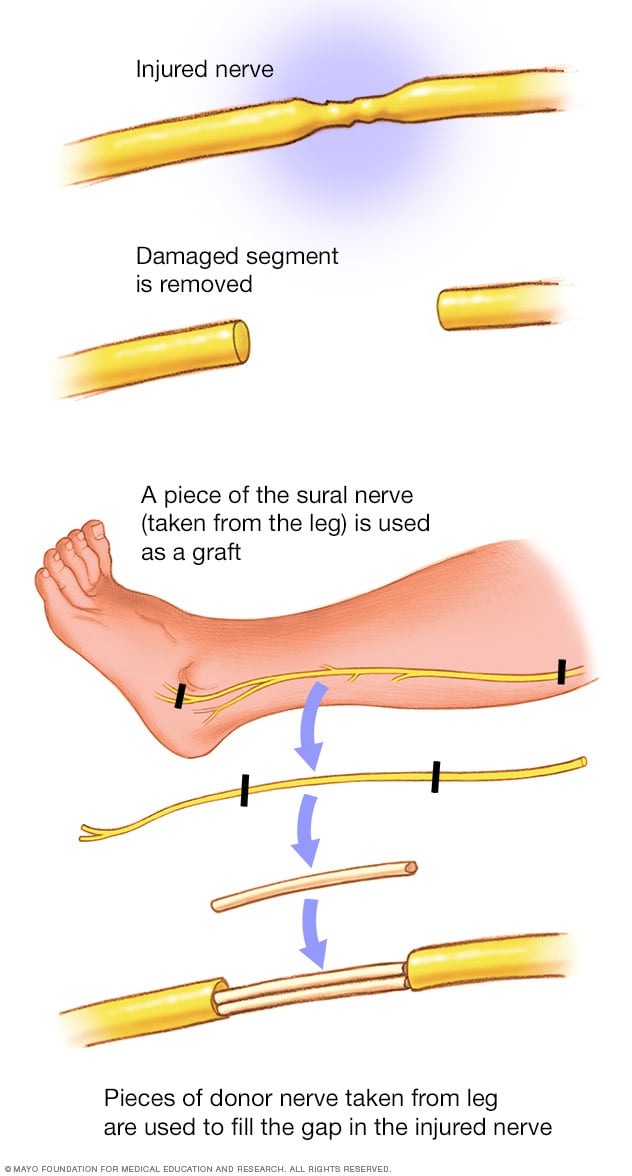
Peripheral nerve graft
To repair a damaged nerve, a surgeon removes a small part of the sural nerve in the leg and implants this nerve at the site of the repair.
Sometimes the surgeon can use another working nerve to make an injured nerve work, known as nerve transfer.
Peripheral nerve transfer
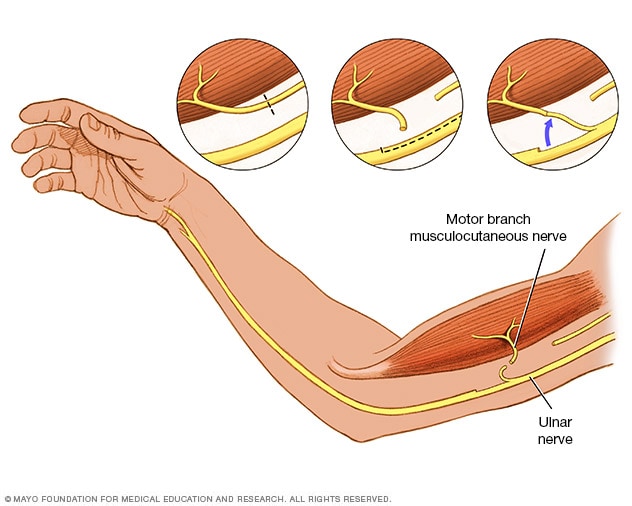
Peripheral nerve transfer
Your surgeon can bypass a damaged section of nerve by connecting a healthy nerve to restore function.
If you have a serious nerve injury, surgery can restore function to critical muscles by transferring tendons from one muscle to another.
Restoring function
A number of treatments can help restore function to the affected muscles.
- Braces or splints. These devices keep the affected limb, fingers, hand or foot in the proper position to improve muscle function.
- Electrical stimulator. Stimulators can activate muscle served by an injured nerve while the nerve regrows. However, this treatment may not be effective for everyone. Your healthcare professional can discuss electrical stimulation with you if it's an option.
- Physical therapy. Therapy involves specific movements or exercises to keep affected muscles and joints active. Physical therapy can prevent stiffness and help restore function and feeling.
- Exercise. Exercise can help improve muscle strength, maintain range of motion and reduce muscle cramps.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Preparing for your appointment
Many tests may be used to help diagnose the type and severity of peripheral nerve injury. When you make your appointment, be sure to ask whether you need to prepare for these tests. For instance, you may need to stop taking certain medicines for a few days or avoid using lotions the day of the test.
If possible, take along a family member or friend. Sometimes it can be difficult to absorb all the information you're given during an appointment. Someone who accompanies you may remember something that you forgot or missed.
Other suggestions for getting the most from your appointment include:
- Write down all your symptoms, including how you were injured, how long you've had your symptoms and whether they've gotten worse over time.
- Make a list of all medicines, vitamins and supplements that you take.
- Ask questions. Children and adults with peripheral nerve injuries have several options for restoring lost function. Be sure to ask about all the treatments available to you or your child. If you run out of time, ask to speak with a nurse or have your healthcare professional call you later.