Diagnosis and tests
Because MASLD typically causes no symptoms, it is often found when tests done for other reasons point to a liver condition. For example, a blood test done during a yearly exam may show high levels of liver enzymes, which can prompt more testing that leads to a MASLD diagnosis.
Tests done to diagnose MASLD, rule out other diseases and see how bad the liver damage is include:
Blood tests
- Liver enzyme and liver function tests.
- Complete blood count.
- Iron studies, which show how much iron is in the blood and other cells.
- Tests for chronic viral hepatitis, which includes hepatitis B and hepatitis C.
- Celiac disease screening test.
- Measurement of fasting blood sugar.
- A1C test, which shows how stable your blood sugar is.
- Lipid profile, which measures blood fats such as cholesterol and triglycerides.
Imaging procedures
Imaging tests used to diagnose MASLD include:
- Abdominal ultrasound, which is often the first test used when liver disease is suspected.
- Magnetic resonance imaging (MRI) or computerized tomography (CT) scanning. These tests are better at finding excess liver fat and cirrhosis.
- Transient elastography, a newer type of ultrasound that measures the stiffness of the liver. Liver stiffness is a sign of scarring, also called.
- Magnetic resonance elastography, which combines MRI with sound waves to create a visual map, also called an elastogram, showing the stiffness of body tissues.
Liver biopsy
If other tests show signs of MASH, or if your test results are unclear, your healthcare professional may suggest a liver biopsy. Liver biopsy is a procedure to remove a small piece of tissue from your liver. It is usually done using a needle passed through the abdominal wall. The tissue sample is looked at in a lab for signs of inflammation and scarring. Liver biopsy is a way to diagnose MASH and find out the amount of liver damage, but in most people, noninvasive imaging tests are used instead.
You may feel some discomfort with a liver biopsy, and it does have risks that your healthcare team talks about with you in detail.
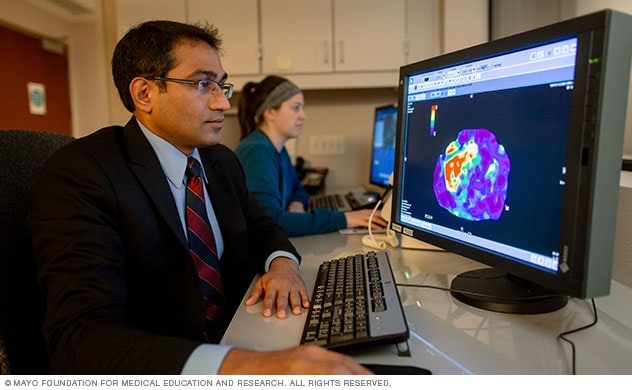
A Mayo Clinic radiologist views a magnetic resonance elastogram of the liver showing areas of scarring, or fibrosis, in red.
More Information
Treatment
Treatment for MASLD usually starts with weight loss. This can be done by eating a healthy diet, limiting portion sizes and exercising. Losing weight may improve other health conditions that can lead to MASLD. Typically, losing 10% of your body weight or more is recommended. But losing even 3% to 5% of your starting weight can have benefits.
Two medicines are available to treat people who have MASH with moderate to severe liver scarring. Resmetirom (Rezdiffra) and semaglutide can help reduce the amount of fat and scarring in the liver. These medicines are not recommended for people with cirrhosis. People who have cirrhosis due to MASH may need a liver transplant.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Self-care
With help from your health care team, you can take steps to manage nonalcoholic fatty liver disease. You can:
- Lose weight. If you're overweight or obese, reduce the number of calories you eat each day and increase your physical activity to lose weight slowly. Eating fewer calories is key to losing weight and managing this disease. If you tried to lose weight in the past and couldn't, ask your health care team for help.
- Choose a healthy diet. Eat a healthy diet that's rich in fruits, vegetables and whole grains. Your health care team may suggest avoiding or limiting certain foods and drinks, such as white bread, red and processed meats, juices, and sweetened drinks. Keep track of all calories you take in.
- Exercise and be more active. Aim for at least 150 minutes of exercise a week. If you're trying to lose weight, you might find that more exercise is helpful. But if you don't already exercise regularly, get your health care team's OK first and start slowly.
- Manage your diabetes. Follow your health care team's advice to manage your diabetes. Take your medicines as told by your care team and watch your blood sugar closely.
- Lower your cholesterol and blood pressure. Improve your cholesterol levels and blood pressure if they are high. A healthy diet, exercise and medicines can help keep your cholesterol, triglycerides and blood pressure at healthy levels.
- Protect your liver. Avoid things that could harm your liver health. For example, don't drink alcohol. Follow the instructions on all medicines and nonprescription drugs. Check with your health care team before using any herbal supplements, as some can harm the liver.
Alternative medicine
No alternative medicine treatments are proved to cure MASH or MASLD. But researchers are studying whether some supplements or natural compounds could be helpful, such as:
-
Vitamin E. In theory, vitamin E and other vitamins called antioxidants could help protect the liver by lessening or canceling out the damage caused by inflammation. But more research is needed.
Some evidence suggests that vitamin E supplements may be helpful for people with MASLD who don't have type 2 diabetes. Vitamin E supplements are not recommended for people with serious liver scarring or type 2 diabetes. Vitamin E has been linked with a slightly increased risk of heart disease and prostate cancer.
- Caffeinated coffee. Some studies suggest that coffee may benefit the liver by reducing the risk of liver diseases such as MASLD and lowering the chance of scarring. It's not yet clear how coffee may prevent liver damage. But certain compounds in coffee are thought to lower inflammation and slow scar tissue growth.
If you already drink coffee, these results may make you feel better about your morning cup. But if you don't already drink coffee, this probably isn't a good reason to start. Discuss the possible benefits of coffee with your healthcare team.
Preparing for your appointment
See your family or primary healthcare professional first if you have symptoms that worry you. If a liver problem such as MASLD or MASH is suspected, you may be referred to a doctor who specializes in the liver, called a hepatologist.
Because appointments can be short, it's a good idea to be well prepared. Here are a few tips to help you get ready, and what to expect from your healthcare professional.
What you can do
- Know what to do before your visit. When you make the appointment, ask if there's anything you need to do beforehand.
- Write down any symptoms you're having. Include any that may not seem related to the appointment.
- Make a list of all medications, vitamins and supplements you're taking.
- Take any relevant medical records. Examples include the results of any tests you've had that relate to your current condition.
- Take a family member or friend along, if possible. Sometimes it can be hard to remember all the information you get during an appointment. Someone who comes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
If you find out you have MASH or MASLD, some basic questions to ask include:
- Is the fat in my liver hurting my health?
- Will my condition disease become serious?
- What are my treatment options?
- What can I do to keep my liver healthy?
- I have other health issues. How can I best manage them together?
- Should I see a specialist? Will my insurance cover it?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
- Should I plan for a follow-up visit?
In addition to the questions that you've prepared to ask your care team, don't hesitate to ask questions during your appointment.
What to expect from your doctor
Your healthcare professional is likely to ask you a number of questions, such as:
- Have you had any symptoms, such as yellowing of the eyes or skin and pain or swelling around your waist?
- If you've had tests done for these symptoms, what were the results?
- Do you drink alcohol?
- What medicines do you take, including medicines you buy without a prescription and supplements?
- Have you ever been told that you have hepatitis?
- Do other people in your family have liver disease?
Dec. 12, 2025