Diagnosis
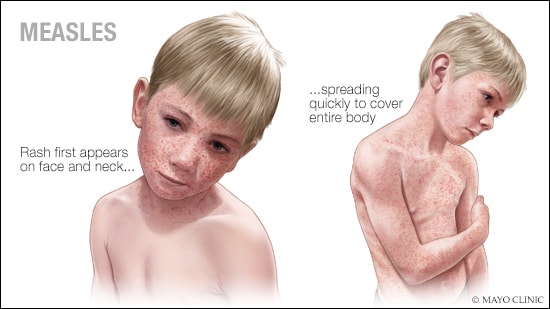
Measles may be diagnosed by a healthcare professional based on the disease's rash as well as tiny white spots inside the mouth, called Koplik spots. The healthcare team may ask whether you or your child has had the measles vaccine, traveled to places where measles is spreading or been around anyone with a rash or fever.
Lab tests can confirm that a person has measles. These tests may look for genetic evidence of the virus or proteins used in the body's response to the virus. To test for measles, your healthcare professional may use a swab to collect a sample from your nose or throat. You also may be asked to give a urine or blood sample.
Treatment
There's no antiviral treatment for measles. But other kinds of well-researched treatments can help ease symptoms, lower the risk of complications and prevent death from measles.
Care options after measles exposure
If people older than 6 months of age are exposed to measles and are not immune by previous illness or vaccination, they can get a measles vaccine for up to three days after contact with the virus. After the vaccine you don't need to stay home, also called quarantine.
For up to six days after exposure, children up to 11 months old who are exposed to measles and are not immune by previous illness or vaccination can get a shot of proteins, called antibodies, that help the body clear an infection. This shot is called immune globulin. After immune globulin treatment, you do need to quarantine for 21 days.
Measles care tips
Get plenty of rest and eat nutritious foods as you're able. To help prevent fluid loss, called dehydration, focus on drinking fluids. Water, broth or drinks with minerals, called rehydration solutions, may help replace fluids. Talk with your healthcare professional before giving rehydration fluids to infants.
For fever with achiness, medicines available without a prescription may help. Read the labels carefully or ask your healthcare professional or pharmacist about the right dose. Do not give aspirin to children or teenagers. Aspirin has been linked to Reye's syndrome, a rare, life-threatening condition, in children and teenagers who have the flu or chickenpox.
Care for measles complications
If you get a bacterial infection, such as pneumonia or an ear infection, with the measles, you might need an antibiotic. But antibiotics don't treat measles.
Measles can lead to inflammation of the airways. The inflammation lowers the body's ability to take in oxygen. If this happens, you may need extra oxygen or breathing help.
A healthcare professional may give children vitamin A as part of treatment for measles. The dose of vitamin A depends on the child's age. Children with low levels of vitamin A who get measles are more likely to be very sick than are children with recommended levels.
Vitamin A supplements do not prevent measles. Getting a measles vaccine is the most effective and safest way to prevent measles. Children should not be given vitamin A as a treatment or supplement unless recommended by a healthcare professional. If a vitamin A supplement is recommended, take only the recommended amount. Taking too much vitamin A can cause major harm.
These treatments are well researched and help people with measles feel better, manage complications and prevent death.
Other treatments with limited evidence
Other treatments for measles may have serious side effects and limited supporting evidence. For example, there is no clear benefit of steroid treatments of any kind. Steroid treatment may make measles worse in some people. In other situations, treatment may help only people at high risk of serious measles illness or those who are already very ill. A qualified healthcare professional can help you understand the risks and benefits based on your situation.
History of infectious disease outbreaks and vaccines timeline.
Learn about the history of major disease outbreaks, epidemics and pandemics, as well as the impact vaccines and research had on many infectious diseases.
Find out more at History of infectious disease outbreaks and vaccines timeline.
Preparing for your appointment
If you suspect measles, make an appointment with your healthcare professional. When you get to the medical office, be sure to tell the staff at the check-in desk that you suspect measles. You and your child likely will be asked to wear a face mask and should be taken to an exam room right away.
What you can do
Before your appointment, make a list of:
- Symptoms and when they began.
- Key personal information, including recent travel or contact with someone who was sick.
- All medicines, vitamins or supplements that you or your child takes, including doses.
- Questions to ask your healthcare professional.
Some basic questions to ask include:
- What's the most likely cause of these symptoms?
- What are other possible causes?
- How can I make my child more comfortable?
What to expect from your doctor
Your healthcare professional may ask that you come in before or after office hours to lower the risk of spreading measles. Also, if you or your child has measles, the healthcare professional must report the illness to the local health department.
Be ready to answer questions such as:
- Have you or your child been vaccinated against measles? When?
- Have you traveled out of the U.S. recently?
- Do others live with you? Have they been vaccinated against measles?
What you can do in the meantime
Before the appointment:
- Rest
- Drink lots of fluids.
- Stay away from others.