نظرة عامة
NF2-related schwannomatosis (NF2) is a rare genetic condition. It causes tumors to grow on the hearing and balance nerves, most often in both ears, which can lead to hearing loss. The gene change that causes the tumors can be inherited from a parent. Or the gene change can happen spontaneously. That means it happens for the first time and isn't passed down from a parent.
The condition was previously called neurofibromatosis type 2. The condition itself has not changed — only the name. It causes tumors to grow on the hearing and balance nerves in both ears. These tumors are called vestibular schwannomas. They are not cancer. The tumors can lead to hearing loss or balance problems. People with NF2 also may develop other noncancerous tumors on the brain, spine or nerves. These tumors can include meningiomas, other schwannomas or ependymomas in the spinal cord.
NF2-related schwannomatosis is one type of schwannomatosis, a group of conditions where schwannomas can form in different parts of the body. Schwannomas are noncancerous tumors that start in the cells covering nerves.
NF2 is not cancer. But they can still cause problems by pressing on nearby nerves or the brainstem. Because of this, regular imaging and hearing checks are important. Treatment may include radiation, surgery or targeted medicines such as bevacizumab.
NF2 is rare. It affects about 1 in 60,000 people. Many people have no family history of NF2. Some have mosaic NF2, which means only some cells carry the gene change. This can lead to milder symptoms or symptoms that start later in life.
NF2-related schwannomatosis is different from neurofibromatosis type 1 (NF1). NF1 often begins with skin changes like cafe au lait spots and freckling, and may include neurofibromas, learning differences and optic pathway gliomas. NF2 causes tumors on the hearing and balance nerves that can lead to hearing loss, tinnitus and balance problems, along with other brain or spine tumors. Skin changes in NF2 are usually mild.
Neither type of neurofibromatosis is considered worse. Effects vary from person to person based on which tumors are present, how fast they grow and the symptoms that develop. With careful monitoring, timely treatment and support for hearing and balance, many people live full lives with NF2.
الأعراض
NF2-related schwannomatosis, previously called neurofibromatosis type 2 or NF2, causes symptoms that usually result from slow-growing tumors in both ears. These tumors are known as vestibular schwannomas. They also are called acoustic neuromas. These tumors are benign, which means they are not cancer.
The tumors grow on the nerve that carries sound and balance information from the inner ear to the brain. Because of this, one of the first signs of NF2 is hearing loss in one or both ears. Ringing in the ears and balance problems also are common early symptoms.
While NF2 mostly affects the nerves that control hearing and balance, tumors in other parts of the brain can sometimes affect nearby areas that help with coordination or movement. However, NF2 usually does not directly affect thinking, memory or the hypothalamus, which controls hormones and body functions.
Symptoms often begin in the late teen or early adult years, when tumors start to cause changes in hearing, balance or vision.
Symptoms of NF2 depend on where tumors grow. Common symptoms include:
- Gradual hearing loss.
- Ringing in the ears.
- Poor balance or unsteadiness.
- Headaches.
Some people with NF2 may have small skin lumps or bumps. These are usually caused by tumors growing on nerves under the skin. These lumps and bumps are different from the skin changes seen in other types of neurofibromatosis.
Sometimes NF2 can cause visible changes in the face. Facial muscles may become weak or droop if tumors grow on the facial nerve, which controls movement of the face. This may make it harder to smile, blink or move facial muscles on one side.
NF2 also can lead to the growth of tumors on other nerves, including in the brain, spine and eyes. Tumors also may grow on peripheral nerves, which are outside the brain and spinal cord. People who have NF2 may develop other benign tumors as well.
Symptoms from tumors in other areas may include:
- Numbness and weakness in the arms or legs.
- Pain.
- Poor balance.
- Facial droop.
- Changes in vision or cataracts.
- Seizures.
- Headaches.
الأسباب
NF2-related schwannomatosis is caused by a change, called an alteration, in the NF2 gene on chromosome 22. This gene makes a protein called merlin. Merlin also is known as schwannomin. It helps control cell growth and prevent tumors. When the gene is altered, the body does not make enough merlin. Without merlin, cells can grow when they should not. This can lead to tumors forming on nerves.
Role of genes and inheritance
For about half of people who have NF2-related schwannomatosis, the altered gene is inherited from a parent. NF2 follows an autosomal dominant inheritance pattern. This means that any child of an affected parent has a 50% chance of having the gene change.
The other half of people with NF2 develop the condition because of a new gene change, called a de novo mutation. This means that neither parent has the gene change. The gene change occurs for the first time in that person.
Mosaic NF2
Sometimes, the gene change occurs in only some of the body's cells. This is called mosaic NF2. People with mosaic NF2 may have milder symptoms or develop them later in life. Because not all cells carry the gene change, the chance of passing NF2 to a child may be lower than 50%.
These gene changes explain why NF2-related schwannomatosis is a condition passed down in families. It is not caused by lifestyle or environmental factors.
عوامل الخطورة
نمط وراثي صبغي جسدي سائد
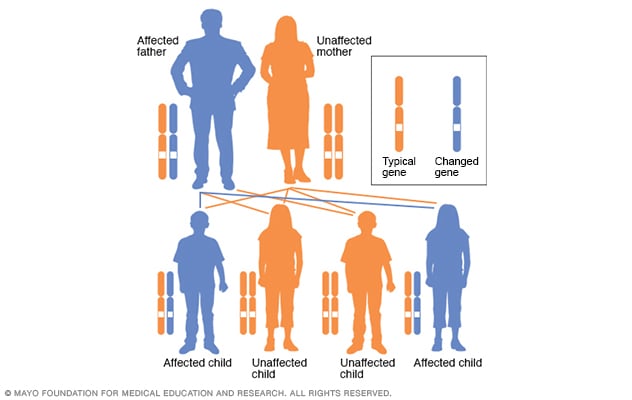
نمط وراثي صبغي جسدي سائد
في نمط الوراثة الجسدي السائد، يكون الجين المتحور جينًا سائدًا. ويوجد في أحد الصبغيات (الكروموسومات) اللاجنسية التي تُسمى الصبغيات الجسدية. ولا يحتاج الأمر سوى جين متحور واحد لإصابة الشخص بهذا النوع من الحالات. وهناك احتمال بنسبة 50% أن يولد طفل مصاب بجين متحور واحد واحتمال بنسبة 50% أن يولد طفل سليم للشخص المصاب بحالة اضطراب الصبغي الجسدي السائد، وهو الأب في هذا المثال.
For about half of people who have NF2-related schwannomatosis, the altered gene is passed down from a parent. NF2 has an autosomal dominant inheritance pattern. This means any child of an affected parent has a 50% chance of having the gene change. The other half of people with NF2 develop the condition because of a new gene change that was not present in either parent.
Having a family history of NF2 is the only known risk factor. NF2 occurs in people of all backgrounds and regions at similar rates. There are no known geographic or ethnic factors that increase risk.
المضاعفات
NF2 affects many parts of the body because it causes tumors to grow on nerves throughout the brain and spinal cord. NF2 complications vary by which nerves or parts of the brain or spine are involved.
Sensory and communication complications
- Partial or total hearing loss.
- Balance trouble or dizziness.
- Vision changes, including cataracts.
- Speech or swallowing difficulty.
Physical and nerve complications
- Numbness, tingling or weakness in an arm or leg.
- Small skin schwannomas that may cause pain or affect appearance.
- Multiple benign brain or spine tumors that can press on the brain or spinal cord.
- Chronic pain or headaches.
Treatment and emotional complications
- Side effects after treatment, such as hearing decline after surgery or radiosurgery and rare radiation-related tumor effects.
- Emotional stress, anxiety or depression.
- Communication challenges from hearing loss.
How NF2 affects the body beyond hearing loss
NF2 tumors can press on nearby structures in the brain or spinal cord and affect movement, vision, swallowing or balance. Tumors on the spinal nerves can cause numbness, weakness or pain in the arms or legs. Meningiomas may form on the surface of the brain or spine and increase pressure inside the skull, leading to headaches or seizures. Cataracts and other eye problems also are common. Over time, these issues can affect mobility, independence and quality of life. These complications can vary in severity and may change over time.
Because complications can vary, the long-term outlook depends on where and how tumors grow.
Life expectancy with NF2
Life expectancy varies widely. It depends on the number, size and location of tumors. It also depends on how early the condition is diagnosed and treated. Many people with NF2 live into middle or late adulthood, especially with regular monitoring and modern treatments that preserve hearing and nerve function. Advances in MRI techniques, microsurgery and targeted medicines have improved outcomes and helped people maintain a longer, higher quality life.
NF2 is not cancer. But its tumors can cause serious complications if they press on vital areas of the brain or spinal cord. These problems can be life-threatening in some cases, especially without monitoring or treatment.
Recurrence or regrowth of tumors
NF2-related tumors, especially vestibular schwannomas and meningiomas, can grow back after surgery. Complete removal can be difficult if tumors are close to vital nerves or brain structures. Even after successful surgery, new tumors may appear in other areas over time because the underlying genetic change remains in the body's cells. Ongoing MRI scans, hearing tests and neurological exams are important to find and manage new or recurrent growth early.