概述
前列腺切除术是一种切除部分或全部前列腺的手术。前列腺是男性生殖系统的一部分,位于骨盆内的膀胱下方。前列腺环绕着称为尿道(将尿液从膀胱输送到体外)的空心管道。
前列腺切除术是治疗前列腺癌的常见手术,也可以治疗累及前列腺的其他医疗状况。可能会进行不同类型的前列腺切除术,具体取决于需要治疗的医疗状况。
类型
根治性前列腺切除术是一项切除整个前列腺及周围一些组织的手术。该手术用于治疗前列腺癌。有时还会切除附近的淋巴结。
- 开放式根治性前列腺切除术。 在这种传统开放式手术中,外科医生仅通过一个长切口切除前列腺。
- 开放式根治性耻骨后前列腺切除术。 这是一种经由下腹部长切口进行的开放式根治性前列腺切除术。
- 开放式根治性经会阴前列腺切除术。 这是一种在肛门与阴囊中间部位做长切口进行的开放式根治性前列腺切除术。手术部位称为会阴。这种手术并不常做,因为它更有可能引起勃起问题,而且无法切除淋巴结。但与经耻骨后入路相比,这种手术造成的疼痛可能更少,术后更容易恢复。
- 根治性腹腔镜前列腺切除术。 在这种类型的手术中,经由下腹部几个小切口(而非大切口)插入工具来切除前列腺。目前,这种手术方法比开放式手术更常见,并且通常在机器人辅助下进行。由于这种手术在下腹部进行,因此也被视为经耻骨后入路。
- 机器人辅助根治性腹腔镜前列腺切除术(RALP)。 机器人前列腺切除术是一种常见的腹腔镜手术。外科医生坐在控制面板(控制台)前,并用其移动连接至机械臂的手术工具。手术工具通常经由几个下腹部小切口插入。由于该手术在下腹部进行,因此也被视为经耻骨后入路。在较少情况下,该手术经由会阴部较大切口完成,也被视为经会阴入路。外科医生可通过机器人前列腺切除术进行精细操作。因此,与开放式手术相比,机器人前列腺切除术引起的疼痛和出血可能较少。术后恢复时间也可能更短。
- 保留神经的前列腺切除术。 在这项手术中,外科医生会采用上述手术方法中的一种切除前列腺,同时尽量避免损伤在勃起中起作用的神经。如果癌灶非常靠近神经,则可能无法进行这项手术。在这种情况下,可能需要进行不保留神经的前列腺切除术。
单纯前列腺切除术有时也称为部分前列腺切除术,是一项切除前列腺大部分内部组织的手术。它会完整保留前列腺的外层组织。经常使用该手术为良性前列腺增生(BPH)(一种前列腺严重肿大的医疗状况)缓解症状。单纯前列腺切除术通常采用腹腔镜和机器人辅助方法,经由下腹部小切口完成。由于这种手术在下腹部进行,因此也被视为经耻骨后入路。单纯前列腺切除术可能采用以下方式进行:
- 腹腔镜单纯前列腺切除术。
- 机器人辅助单纯前列腺切除术。
- 开放式单纯前列腺切除术。
妙佑医疗国际的泌尿科医生使用先进的内镜技术解决前列腺肿大症状,在大多数情况下无需进行开放式、腹腔镜或机器人手术。
手术团队将与您讨论每种技术的优缺点。您还可以提出自己的偏好。您将和手术团队一起决定最适合您的方法。
目的
前列腺切除术可能用于治疗前列腺癌,也可能用于治疗前列腺肿大,这是一种称为良性前列腺增生(BPH)的医疗状况。
因癌症切除前列腺
大多数情况下,前列腺切除术用于治疗可能尚未扩散至前列腺以外的癌症。医生将切除整个前列腺及周围的一些组织,这种手术称为根治性前列腺切除术。该手术可以单独采用,也可以与放疗或激素治疗等其他治疗方法联合采用。
减轻 BPH 的症状和并发症
为治疗 BPH,外科医生会切除前列腺的大部分内部组织,这被称为单纯或部分前列腺切除术。对于一些患有严重泌尿系统症状和前列腺肿大的患者,这可能是一种治疗选择。
该手术可减轻因尿流阻塞而引起的泌尿系统症状和并发症,例如:
- 尿频尿急。
- 排尿困难。
- 排尿缓慢(排尿时间长)。
- 夜间排尿次数多于平时。
- 排尿断断续续。
- 无法完全排空膀胱的感觉。
- 尿路感染。
- 无法排尿。
 解释前列腺切除术的方案
解释前列腺切除术的方案
妙佑医疗国际的泌尿科医生在解释前列腺切除术的方案。
风险
您可能想知道,如果没有前列腺,您是否能够生存或生活。答案是肯定的。像任何手术一样,前列腺切除术也存在一些风险和副作用。医护团队会尽力降低这些风险。
根治性前列腺切除术的风险和副作用
根治性前列腺切除术的风险和副作用包括:
- 出血。
- 血凝块。
- 丧失排尿控制功能(也称为尿失禁)。随着时间的推移,此症状通常会消退。
- 无法达到并保持足够坚挺的勃起以进行性交(又称为勃起功能障碍)。
- 将尿液排出身体的管道(称为尿道)变窄。或者膀胱颈部(尿道和膀胱连接部位)变窄。
- 淋巴积液。
- 极少情况下出现大肠或直肠损伤。
术后几周内,疼痛是常见症状。医护团队会与您一起制定疼痛控制方案。
与开放式前列腺切除术相比,机器人前列腺切除术可以减少出血和疼痛,缩短住院时间,并加快恢复。
妙佑医疗国际的泌尿科医生接受过实施前列腺切除术的高级培训,在手术的各个方面都具备丰富经验。这些专业技能的积累很大程度是因为治疗过大量患者。妙佑医疗国际做过大量手术、临床试验和先进治疗,因此能为接受护理的患者提供最佳护理体验。此外,妙佑医疗国际的方案基于对前列腺解剖结构的深度了解,治疗过程注重保留排尿控制功能和性功能。综合性人性化护理方案重视生理预后和生活质量,令患者受益。这种方式确保手术患者的并发症发生率最低并获得最佳预后。
单纯前列腺切除术的风险和副作用
单纯前列腺切除术会切除前列腺的大部分内部组织,对缓解泌尿系统症状效果良好。但与其他创伤性更小的前列腺肿大治疗方法相比,其并发症风险更高,恢复时间也更长。创伤性更小的治疗方法包括经尿道前列腺切除术(TURP)。在 TURP 中,外科医生只切除小部分前列腺组织。该手术通过尿道(将尿液排出体外的管道)进行。创伤性更小的治疗方法还包括选择性激光前列腺汽化术(也称为激光 PVP 手术)和钬激光前列腺剜除术(HoLEP)。
单纯前列腺切除术的风险和副作用包括:
- 出血。
- 血凝块。
- 尿路感染。
- 尿失禁。
- 射精时精液流入膀胱而不是通过阴茎流出体外。这种情况称为逆向射精。
- 勃起功能障碍。
- 开放式手术后尿道或膀胱颈变窄。
术后几周内,疼痛是常见症状。医护团队会与您一起制定疼痛控制方案。
何时就医
预计会出现一些副作用,但有时可能需要就医。
如果发生以下情况,请拨打 911 或当地急救电话:
- 一侧腿部新发疼痛、肿胀、发红、僵硬或麻木感,尤其是在小腿下部。
- 气短。
- 胸部疼痛或黑视。
如果出现以下情况,请致电医护团队:
- 导尿管堵塞、尿量减少或导尿管滑脱。
- 尿液浓稠、呈红色和番茄酱状,或尿液中有小葡萄般甚至更大的血凝块。
- 排尿困难或排尿疼痛。
- 拔除导尿管后排尿无力或超过四小时无法排尿。
如果出现以下情况,请立即致电医护团队:
- 新发疼痛或使用止痛药后疼痛未见缓解。
- 感染迹象,例如:体温达到 38 摄氏度(100.4 华氏度)或更高;愈发严重的疼痛、压痛或肿胀;引流液有臭味或切口周围肤色发生变化。这种变化可能是发红、发紫或发黑,具体取决于肤色。
- 尿液气味发生很大变化。
- 手术结束后几天内,导尿管周围每天多次出现渗漏。如果导尿管周围渗漏的尿液量多于流入引流袋的尿液量,也请致电医护团队。
- 膀胱痉挛、下背部(脊柱两侧肋骨正下方)痛性痉挛或淤伤。
- 切口边缘裂开。
- 胃部不适或呕吐。
如何进行准备
术前,外科医生可能会进行一次膀胱镜检查。这项检查使用一种称为内窥镜的设备来观察您的尿道和膀胱内部。通过膀胱镜检查,外科医生可查看您的前列腺大小,并检查泌尿系统。外科医生可能还会要求做其他检查,包括血液检测或测量前列腺和尿液流量的检查。
术前,请谨遵外科医生团队的医嘱行事。
饮食和用药
与医护团队讨论以下事项:
- 您的药物。 告知手术团队您使用的任何药物或补充剂,无论是否需要处方。如果您使用华法林(Jantoven)或氯吡格雷(Plavix)等血液稀释药物,请务必告知医护团队。如果您使用一些非处方止痛药,也请务必告知医护团队。例如,如果使用阿司匹林、布洛芬(Advil、Motrin IB 等)或萘普生钠(Aleve)等,请告知医护团队。外科医生可能会要求您在手术前几天停用那些增加出血风险的药物。
- 药物过敏或反应。 告知手术团队您出现过的任何药物过敏或反应。
- 术前禁食。 外科医生可能会要求您在午夜之后禁食禁饮。在手术当日早晨,只用一小口水送服外科医生要求您服用的药物。
- 术前肠道准备。 手术前,医生会给您一套工具并提供操作说明,帮助您清理肠道。
衣物和个人物品
做好计划,避免在手术期间佩戴以下物品:
手术后的安排
请询问外科医生您需要住院多长时间。请提前安排他人开车送您回家。术后您无法立即开车。
活动限制
在手术后的几周内,您可能无法工作或做剧烈活动。请询问外科医生,了解您需要多长时间才能恢复。
可能出现的情况
术前
前列腺切除术通常会使用药物来止痛,并使您处于类似睡眠的状态。这称为全身麻醉。外科医生也可能会在手术前给您开具抗生素,避免出现细菌感染。
术中
前列腺切除术切口
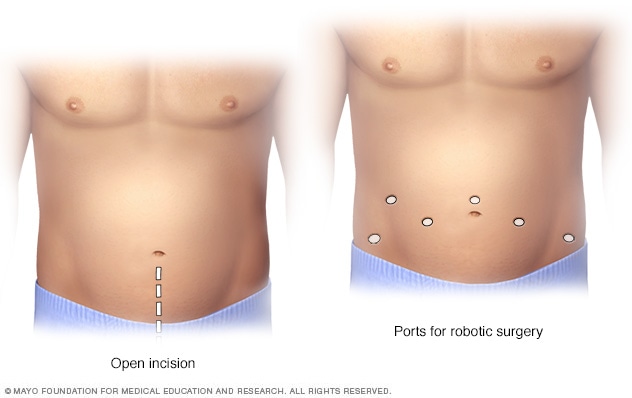
前列腺切除术切口
在开放式前列腺切除术中,医生会在下腹部做一个大切口(左图)。而机器人前列腺切除术则需要在腹部开几个较小的切口(右图)。
在前列腺切除术中如何切除前列腺以及切除多少前列腺组织,取决于个人情况和所采用的具体手术。例如:
-
机器人辅助根治性前列腺切除术。 这种类型的手术使用微型管状摄像头和小型机器人工具完成,这些工具经由几个腹部小切口插入。一名外科医生坐在控制面板(控制台)前。控制台离您和手术台很近。外科医生精准地控制机器人工具的移动。这些工具经过专门设计,具有与人类手部、手腕和手指相似的活动度。
控制台会显示手术部位的放大三维视图。与传统腹腔镜手术相比,这种方式让外科医生能够更清晰地观察手术过程。机器人系统让外科医生能够进行更小、更精确的切口。与传统开放式手术相比,这能帮助一些患者更快地恢复。机器人辅助手术也可减少某些并发症。
- 开放式根治性前列腺切除术。 外科医生会在下腹部(从肚脐以下到耻骨上方)做一个切口,将前列腺与周围的神经和血管仔细分离,然后切除前列腺及邻近组织,并用缝合线缝合切口。
-
单纯前列腺切除术。 开始手术时,外科医生可能会在阴茎前端插入一个细长柔性观察镜(膀胱镜),以便能够看清尿道、膀胱和前列腺区域的内部情况。然后,外科医生会将一根管子(导管)插入阴茎前端,导管进入膀胱,用于在手术期间引流尿液。做切口的部位取决于外科医生所采用的技术。
外科医生把引起症状的前列腺部分切除后,可能插入 1 至 2 根引流管。通过在手术部位附近经皮穿刺置管。一根引流管直接插入膀胱。另一根则插入前列腺切除部位。过一段时间后拔除引流管。
在手术室内进行前列腺切除术所需的时间会有所不同。不过一般来说,这项手术需要两到四个小时。其中不包括术前准备时间或术后在恢复区的留观时间。所有环节总共可能需要半天到一天的时间。
术后
术后,您可能需要:
- 使用止痛药。可能接受静脉注射(IV)给药,也可能口服处方止痛药。
- 行走。 您可能需要在手术当日或次日行走。
- 在术后 1 到 2 天回家。 如果外科医生认为您可以安全回家,则可能会为您拔除盆腔引流管(如有)。一到两周后,您需要到外科医生处复诊拆线。
- 回家时留置导尿管。 大多数患者在术后 7 至 14 天需要使用导尿管。
常见问题包括:
- 我需要何时以及多久一次前往医疗护理专业人员处复诊以确保一切正常? 前列腺切除术后,您可能需要在两周后以及 6 至 8 周后前往医疗护理专业人员处复诊。之后前往医疗护理专业人员处复诊的频率取决于您的健康状况以及接受前列腺切除术的原因。例如,如果因癌症切除前列腺,您可能需要在术后第一年内每几个月接受一次前列腺特异性抗原(PSA)血液检测。请向医疗护理专业人员咨询最适合您的复诊频率。
-
前列腺切除术后多久能恢复? 每个人的恢复时间不同,但多数会在大约 4 至 6 周内恢复正常。在进行特定活动时可能与以前有所不同。请确保您了解术后需要采取的自我护理措施。例如,请勿穿戴紧身衣物或松紧腰带,因为这可能会在伤口愈合期间刺激皮肤。您通常可以恢复正常饮食。
可能要求您在术后戒酒数天或更长时间,直至您停用任何处方止痛药。了解需要遵循的任何限制,例如开车或提举重物的限制。
-
恢复期间有哪些典型的活动限制? 请向医护团队咨询适合您的活动限制。上下楼梯和简单家务通常没有问题。至少四周内不要提举超过 4.5 公斤(10 磅)的物品。另外,至少在四周内不要进行涉及弯腰、推拉、扭身或俯身动作的剧烈活动。在拔除导尿管且征得医护团队同意前,请勿驾车或操作机器。
您可能需要在数月内避免进行需要采用跨坐姿势的活动,例如驾驶摩托车和坐在单车上。请在恢复性活动前咨询医疗护理专业人员。
在恢复期间,走路是最好的运动方法。慢慢开始,例如可以每天几次、每次走几分钟。等您感觉准备好了,再逐渐加量。
- 在前列腺切除术后出现睾丸肿胀是正常现象吗? 睾丸不会肿胀。但大腿和阴囊(包裹睾丸的结构)可能在术后出现肿胀和淤伤。通常会在几天内消肿。淤伤消退则通常需要几周时间。
- 切除前列腺后,身体会发生什么情况或出现哪些变化? 前列腺手术可能削弱控制排尿的肌肉。这可能导致漏尿。您可能需要使用防护垫或一次性尿布。医护团队可能会向您告知有助于在拔除导尿管后增强膀胱肌肉的锻炼方法。在康复期间,排尿控制功能会得到改善。多数接受前列腺手术的患者会在术后一年内完全恢复膀胱功能。切除前列腺的手术也可能影响勃起功能。
- 切除前列腺会导致阳痿吗? 前列腺切除术可能影响控制性功能的神经。在前列腺切除术后,勃起功能恢复时间会有所不同。有些患者可能立即恢复勃起功能。有些患者可能在使用药物后逐渐恢复勃起功能。受累神经愈合可能需要两年或更长时间。多数患者至少会在一定程度上丧失勃起功能。患者越年轻,所受影响可能越轻。某些较年长的患者术后可能无法恢复性功能。
- 如何管理术后勃起功能障碍? 请在恢复性活动前咨询医护团队。如果您接受了保留神经的手术,医护团队可能给您开治疗勃起功能障碍的药物疗法。这可能包括每周两次使用他达拉非(Adcirca、Cialis 等)或西地那非(Revatio、Viagra)之类的药物。这些药有助于增加生殖器部位的血流量和含氧量。从而促进肌肉和神经愈合。请遵医嘱使用药物,即使您没有尝试进行性交。用药 6 至 12 周后,如果需要,您通常会在性活动前使用一片药物。
- 前列腺切除术后,精液或精子会去哪里? 前列腺切除术会切除前列腺和精囊。这些腺体产生射精时排出的大部分精液。因此,在前列腺手术后,性高潮时通常不会排出精液或只有很少精液。
结果
根治性前列腺切除术
前列腺癌可能在前列腺切除术后再次发生,这称为复发。大约三分之一接受根治性前列腺切除术的患者会在 10 年内复发。因此您需要定期接受 PSA 血液检测。PSA 检测有助于医疗护理专业人员监测是否复发。
如果是为了治疗癌症而切除前列腺,您在术后的 PSA 值应该检测不到。
单纯前列腺切除术
单纯前列腺切除术通常可长期缓解因前列腺肿大引起的泌尿系统症状。这是治疗前列腺肿大的手术中最具侵入性的一种,但很少发生严重的并发症。多数接受该手术的患者无需接受针对 BPH 的任何后续治疗。
临床试验
探索 Mayo Clinic 的研究 测试新的治疗、干预与检查方法,旨在预防、检测、治疗或控制这种疾病。
Jan. 13, 2026