Mayo Clinic's approach
Teamwork
 Pancreas transplant consultation
Pancreas transplant consultation
Pancreas transplant consultation at Mayo Clinic
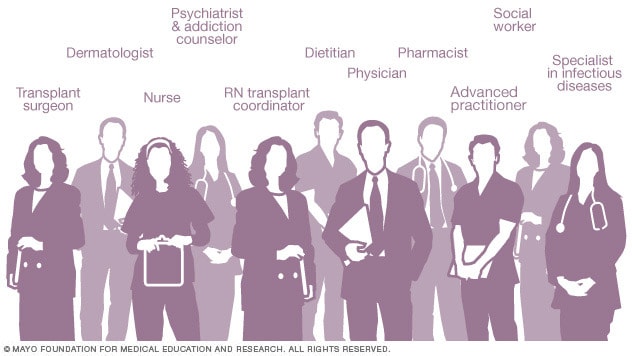
At Mayo Clinic, an integrated team of healthcare professionals trained in endocrinology, abdominal transplant surgery, infectious disease management and other specialties focuses on your needs and the needs of your family before, during and after your pancreas transplant.
Surgeons, doctors, transplant nurses, pharmacists, social workers and others work together to manage every aspect of your pancreas transplant, from planning through post-surgical care.
Coordinated care
 Care team roles
Care team roles
Healthcare professionals trained in many medical specialties work together as a team to ensure positive outcomes after your pancreas transplant.
Having all this subspecialized expertise in a single place, focused on you, means that you're not getting just one opinion. Your care is discussed among the team, your test results are available quickly, appointments are scheduled in coordination, and your transplant care team works together to determine what's best for you.
Surgical expertise
Mayo Clinic surgeons have performed hundreds of successful pancreas transplants using state-of-the-art technology since 1987.
Mayo Clinic is one of only a few transplant centers that offer pancreas transplants to select candidates with type 2 diabetes and treated HIV.
Children also can receive pancreas transplant surgery at Mayo Clinic's campus in Rochester, Minnesota.
Research
At Mayo Clinic, you may have access to clinical trials, research studies and new treatments as part of your care.
Researchers in the Mayo Clinic Transplant Center are actively working to develop new technologies, treatments and techniques to make transplants safer and available to more people.
For example, researchers at Mayo Clinic are developing an artificial pancreas that could greatly improve the quality of life for people with type 1 diabetes and may serve as an alternative to pancreas transplants.
Mayo Clinic researchers also are investigating ways to lower the rejection risk among transplant recipients and seeking new ways to treat people who need transplants of all types.
Read more about the Pancreas Transplant Program at Mayo Clinic.
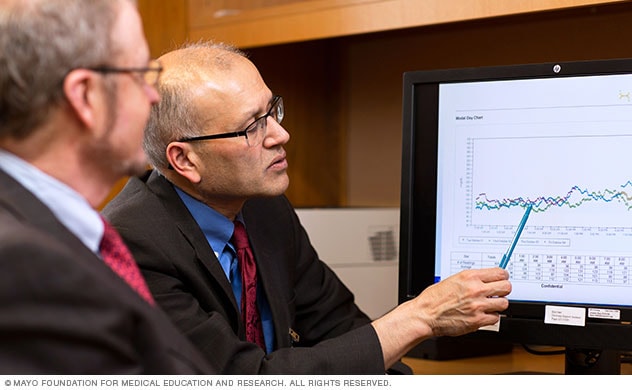
Lowering rejection in organ transplant
Watch Mark Stegall, M.D., and Richard Daly, M.D., discuss lowering rejection risk in organ transplants.
For 12 years, this is the routine that Pete Giannaris has had to accept, kidney dialysis three times a week. As vital as it is, he admits it can wear a guy down.
Pete Giannaris: I mean, even myself, I knew that, man, you know. It has taken a toll on my body.
Pete has dealt with kidney disease most of his life. Even receiving kidney transplants before, but this time was different. He was told he would almost certainly reject any donor organ.
Pete Giannaris: Not many people understand. Oh, you need a kidney. You get on the list. Two years later, you get your kidney and your fine. You know, it's not the story for everybody.
Mark Stegall, M.D. — Mayo Clinic transplant surgeon: About 80 percent of people who have had a previous transplant have antibodies against other tissue types. They also could have been exposed to foreign tissue types by a blood transfusion or even pregnancy.
Anissa Swanigan: I was devastated. Shocked. Didn't really see it coming.
Pregnancy delivered a double-blow to Anissa Swanigan. After giving birth a second time, her weakened heart condition advanced to heart failure and complications scarred her liver so badly it was failing too. Doctors told her she needed a double organ transplant.
Anissa Swanigan: It was the only way you're going to survive.
She had two big reasons to survive. Her two little boys. But, again, high levels of antibodies made her a very poor transplant candidate. Antibodies are a good thing when they help us fight disease. Vaccines, for example, trigger our immune systems to create antibodies. But for some of those waiting to receive life-saving organs, Mayo Clinic transplant surgeon and immunology researcher, Mark Stegall says, antibodies become the enemy.
Mark Stegall, M.D.: It's a big problem. There are about 9,000 people on the kidney transplant list in the United States right now who have really high levels of antibody to the point that they can't really get a transplant.
Pete is in that category, called highly sensitized. So Dr. Stegall and his team did a variety of things in advance to tip the odds in his favor. They carefully selected a living donor for which Pete would have the fewest antibodies. Also, drug researchers found a way to reduce antibody-caused rejection rates from 40% to less than 10%.
Mark Stegall, M.D.: One of the drugs that we were the first to use is a drug called eculizumab. If we give this drug, the antibody binds to the kidney but it doesn't cause the damage.
Pete had also gone through a number of rounds of an antibody filtering process called a plasma exchange. Then, to try to halt the production of new antibodies in his bone marrow, Dr. Stegall turned to an FDA-approved clinical trial at Mayo Clinic using a powerful drug.
Mark Stegall, M.D.: A drug called valcade which is actually used in the treatment of cancers of these antibody-secreting cells. But, of course, these are not cancer cells, these are normal cells.
Anissa also underwent drug and plasma exchange therapies, but her antibody levels were still so high doctors worried that her body might still reject the donor organs.
Richard Daly, M.D. — Mayo Clinic transplant surgeon: By the time the liver went in, the heart might already be irreversibly damaged by the antibodies. So we reversed the process and did the liver transplant first.
Why?
Surgical Director of Heart and Lung Transplantation at Mayo Clinic, Dr. Richard Daly, says the liver filters antibodies. In combined kidney-liver or heart-liver transplants, his team had observed a reduction in antibodies to that donor. However, in multiple organ transplants, hearts generally have to go in first because their tissues are more time sensitive. How does the Mayo team get around that?
Richard Daly, M.D.: Choreograph the whole process. We have to have the donor close enough by. We have to have the procurement done and be really completely ready for the organs when they arrive.
Anissa Swanigan: It seemed brilliant. Brilliant minds that they collaborated and they got together and figured out how to do this thing.
Pete Giannaris: I took a chance. I didn't have anything to lose. So either I stay on dialysis or a miracle happens and I get this kidney.
Innovation that makes a world of difference, one patient at a time.
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.
Expertise and rankings
Experience
 Pancreas transplant teamwork
Pancreas transplant teamwork
Pancreas transplant teamwork at Mayo Clinic
Mayo Clinic has one of the largest transplant practices in the United States. Across its three sites in Minnesota, Florida and Arizona, Mayo Clinic has performed hundreds of successful pancreas transplants. Each year, about 40 people receive pancreas transplants at Mayo Clinic.
Mayo Clinic is one of only a few transplant centers that offer pancreas transplants to select candidates with type 2 diabetes and treated HIV.
Pancreas transplant outcomes at Mayo Clinic compare favorably with the national average.
Innovation and research
Artificial pancreas
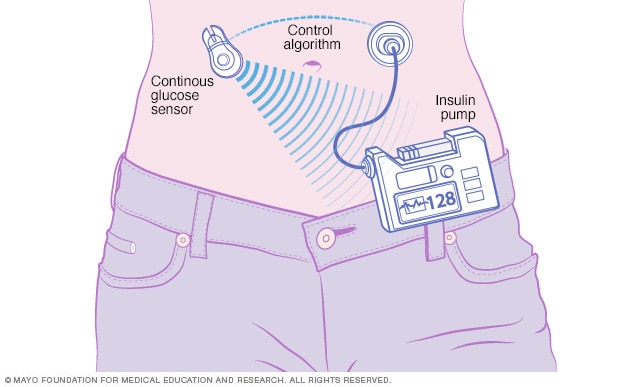
Artificial pancreas
Illustration of artificial pancreas under development at Mayo Clinic
Mayo Clinic surgeons have extensive expertise in many areas of pancreas transplantation, including pancreas-only, combined pancreas-kidney and pancreas-after-kidney transplant.
The Mayo Clinic Transplant Center supports many studies and pancreas transplant research. Mayo Clinic doctors actively research pancreas transplantation techniques and treatment options, presenting their work at national and international meetings.
 Artificial Pancreas Lab
Artificial Pancreas Lab
Artificial Pancreas Lab at Mayo Clinic
For example, researchers at Mayo Clinic are developing an artificial pancreas that could greatly improve the quality of life for people with type 1 diabetes and may serve as an alternative to pancreas transplants.
Mayo Clinic researchers also are investigating ways to lower the rejection risk among transplant recipients and seeking new ways to treat people who need transplants of all types.
Nationally recognized expertise
Mayo Clinic in Rochester, Minnesota, ranks No. 1 for diabetes and endocrinology in the U.S. News & World Report Best Hospitals rankings. Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, are ranked among the Best Hospitals for diabetes and endocrinology by U.S. News & World Report.
Read more about the Pancreas Transplant Program at Mayo Clinic.
Volumes and outcomes
Mayo Clinic's experienced doctors and integrated team approach result in transplant outcomes that compare favorably with national averages. Teams work with transplant recipients before, during and after surgery to ensure the greatest likelihood of superior results.
Volumes and statistics are maintained separately for the three Mayo Clinic locations. Taken together or separately, Mayo Clinic's transplant results are excellent.
Pancreas transplant volumes and statistics
Locations, travel and lodging
Mayo Clinic has major campuses in Phoenix and Scottsdale, Arizona; Jacksonville, Florida; and Rochester, Minnesota. The Mayo Clinic Health System has dozens of locations in several states.
For more information on visiting Mayo Clinic, choose your location below:
Costs and insurance
Mayo Clinic has dedicated transplant financial services representatives and social workers who can assist you with insurance and financial questions regarding your pancreas transplant.
Mayo Clinic works with hundreds of insurance companies and is an in-network provider for millions of people. In most cases, Mayo Clinic doesn't require a physician referral. Some insurers require referrals or may have additional requirements for certain medical care. Many insurance companies require you to get preapproval authorization prior to transplant services.
Read more about pancreas transplant costs and insurance at Mayo Clinic.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Oct. 10, 2025