July 16, 2019
Lacrimal gland biopsy shows extensive reactive lymphoplasmacytic infiltrate
Lacrimal gland biopsy shows extensive reactive lymphoplasmacytic infiltrate
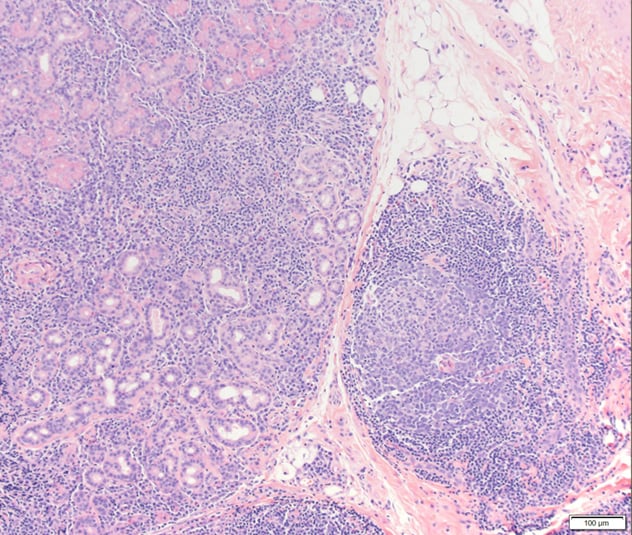
Right lacrimal gland biopsy, hematoxylin-eosin, original magnification times 100 shows extensive reactive lymphoplasmacytic infiltrate.
Lacrimal gland with IgG4-IgG ratio greater than 40 percent
Lacrimal gland with IgG4-IgG ratio greater than 40 percent
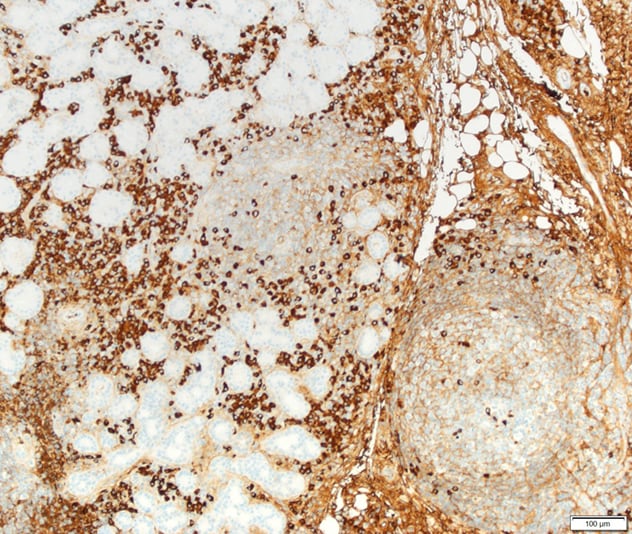
Right lacrimal gland biopsy demonstrates greater than 100 IgG4 staining plasma cells per high-powered field, original magnification times 100. The IgG4-IgG ratio was greater than 40 percent.
Immunoglobulin G4-related ophthalmic disease (IgG4-ROD) is a fibroinflammatory condition characterized by a dense lymphoplasmacytic infiltrate with a preponderance of IgG4+ plasma cells and fibrosis, which was first noted in the pancreas. IgG4 disease was later described as a syndrome, in 2003, when other organ involvement was noted in the patients with IgG4-related pancreatitis. Orbital involvement was first reported in 2007 ― primarily in the form of dacryoadenitis. Subsequent reports describe involvement of the lacrimal gland, orbital soft tissue, extraocular muscles (EOMs) and orbital peripheral nerves. Primary involvement of the EOMs in IgG4-ROD, and lacrimal gland enlargement can lead to diagnostic confusion with Graves' orbitopathy (GO), the most common inflammatory disease of the orbit.
James A. Garrity, M.D., and a research team with Ophthalmology at Mayo Clinic's campus in Rochester, Minnesota, conducted a retrospective, observational study to describe findings among patients with clinical overlap of IgG4-ROD and GO, illustrate the diagnostic challenges, and determine key features that may aid in achieving the correct diagnosis. Results were published in Ophthalmic Plastic and Reconstructive Surgery in 2018.
Diagnosis criteria
Researchers retrospectively identified patients who had diagnoses of GO and IgG4-ROD and were seen in Ophthalmology at Mayo Clinic in Rochester, Minnesota, between June 2009 and November 2013. The team reviewed health records to characterize symptoms, thyroid status, and radiologic, serologic and histologic findings that led to the diagnosis of IgG4-ROD.
Clinical data collected included patient age, sex, race, smoking status, medical history and thyroid-related history, as well as examination findings such as vision, pupils, motility, proptosis, lid retraction or lag, and other signs or symptoms of orbital inflammation. Researchers also collected laboratory values for thyrotropin receptor antibodies, total serum IgG and serum IgG4.
The diagnosis of IgG4-ROD was based on a biopsy and included the number of IgG4+ plasma cells per high-power field (HPF), and the ratio between IgG4+ and IgG+ cells identified by immunohistochemical staining. A finding of 10 or more IgG4 cells per HPF and a ratio of IgG4+-to-IgG+ cells greater than 40 percent were typical findings in the diagnosis of IgG4-ROD.
Among the eight patients (seven male and one female) included in the study:
- Mean age was 46 years.
- Time between diagnoses of GO and IgG4-ROD ranged from one month to eight years.
- Imaging showed enlarged extraocular muscles in all patients.
- Enlarged infraorbital nerves were seen in four patients.
- Tissue biopsy showed CD20+ lymphocytes with a large proportion of IgG4 plasma cells in seven of eight orbital specimens.
- Six patients had a ratio of IgG4-to-IgG cells greater than 40 percent.
Treatment included rituximab in all patients. "Symptoms improved substantially in six patients after rituximab treatment, and two had progression or minimal improvement," says Dr. Garrity. "These two patients were subsequently treated with intravenous corticosteroids and methotrexate, or mycophenolate mofetil, and had symptom resolution."
Patient subgroups
"The eight patients in this study illustrate the clinical overlap of GO and IgG4-ROD, which can lead to confusion for the clinician. Although clinical, laboratory, radiologic and histologic features support each diagnosis, there are no pathognomonic laboratory or clinical findings. GO remains a clinical diagnosis, and IgG4-ROD may be misdiagnosed," says Dr. Garrity.
Researchers separated the eight patients into three groups:
- Patients one and two had a past serologic diagnosis of Graves' disease with orbitopathy (positive thyrotropin receptor antibodies), but the disease did not follow the expected clinical course for GO and they were later found to also have IgG4-ROD.
- Patients three, four, five and six had IgG4-ROD that was initially missed and incorrectly diagnosed as GO.
- Patients seven and eight had presumed GO and IgG4-ROD simultaneously.
"Some key features help distinguish the conditions," says Dr. Garrity. "GO is likely if findings include increased thyrotropin receptor antibodies, lid retraction or lid lag, and a characteristic pattern of enlarged extraocular muscles with typical tendon-sparing morphology. Findings suggestive of IgG4-ROD include a history of asthma and progressive orbital disease in patients with a previous diagnosis of GO, a disproportionately large lateral rectus muscle, and enlarged infraorbital nerves.
"Corticosteroid dependency with noninflamed eyes is not typical of GO and should lead the clinician to consider IgG4-ROD. Histologically, GO does not show fibrosis, and chronic inflammation is minimal compared with that in IgG4-ROD. An increased serum IgG4 level and a biopsy showing greater than 10 IgG4+ plasma cells per high-power field and an IgG4-IgG ratio greater than 40 percent will support the diagnosis of IgG4-ROD.
"GO and IgG4-ROD are complicated inflammatory processes that present diagnostic challenges. We recommend biopsy for patients who do not follow the usual clinical course of GO or have clinical characteristics of IgG4-ROD."
For more information
Tooley AA, et al. Distinguishing IgG4-related ophthalmic disease from Graves orbitopathy. Ophthalmic Plastic and Reconstructive Surgery. 2019;35:170.