Oct. 23, 2018
Achalasia is a primary esophageal motility disorder of unknown cause that is characterized by the incomplete relaxation of the lower esophageal sphincter along with an absence of peristalsis, making swallowing difficult. A number of nonsurgical and surgical options exist for the treatment of achalasia. Traditional surgical approaches include open Heller myotomy, laparoscopic Heller myotomy (LHM) and Heller myotomy performed with fundoplication. A partial fundoplication is done to minimize gastroesophageal reflux disease (GERD), which is relatively common in patients undergoing surgical myotomy.
First presented in 2010, peroral endoscopic myotomy (POEM) has evolved and emerged as an alternative to traditional myotomy for the treatment of all achalasia subtypes and other spastic esophageal disorders.
About the procedure
POEM procedure
POEM procedure
POEM sequence.
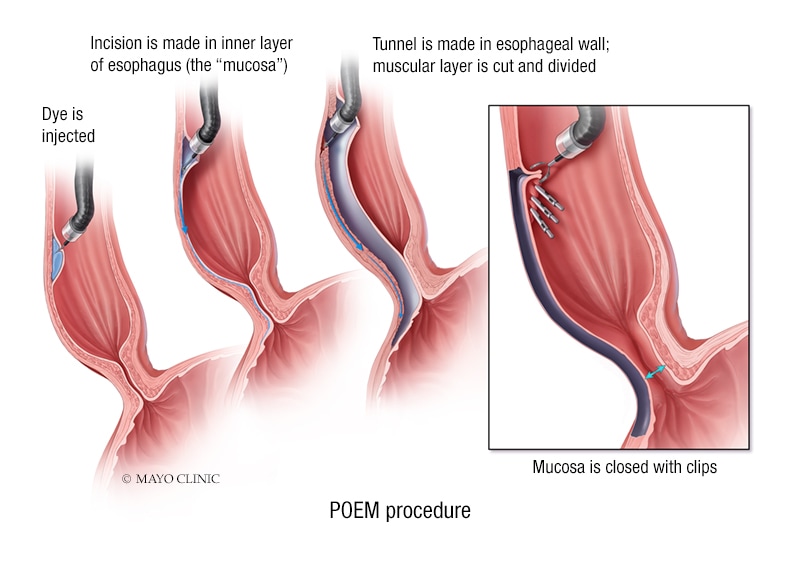
The POEM procedure typically involves the following sequence:
- Mucosal incision
- Submucosal tunneling with dissection
- Myotomy, circular or full thickness
- Closure of mucosal incision
Most endoscopists prefer the use of a cap-fitted, high-definition, diagnostic gastroscope equipped with water jet irrigation. Carbon dioxide, instead of air, provides insufflation throughout the procedure to minimize the risk of gas-related complications. A dye-stained solution is used for submucosal fluid lift prior to mucosal incision and for creation of the submucosal tunnel. Closure of the mucosal incision site is achieved using standard endoscopic clips or a suturing device.
Patients are hospitalized for one to two days after the procedure. An esophagram is typically performed on the following day of the POEM procedure to rule out esophageal leaks and guide diet instructions. A clear liquid diet can be initiated if the esophagram is negative for leaks.
Adverse events
According to Norio Fukami, M.D., a therapeutic endoscopist at Mayo Clinic's campus in Arizona, major complications or serious adverse events (AEs) related to POEM are rare and affect less than 1 percent of patients. These include serious gas-related AEs (for example, tension pneumothorax and tension pneumoperitoneum), mediastinitis, abscess formation and hemorrhage that requires transfusion.
Gas-related events, such as pneumomediastinum and pneumoperitoneum, are common and are an expected occurrence of the procedure. Unless they produce symptoms and require intervention, these events should not be viewed as complications.
POEM versus other treatment modalities
Will POEM become the standard of treatment for achalasia? According to Louis M. Wong Kee Song, M.D., a therapeutic endoscopist at Mayo Clinic's campus in Rochester, Minnesota, several factors associated with POEM make it attractive. These include:
- Control over the length and orientation (anterior or posterior) of the myotomy
- Reduced risk of extraesophageal injury (for example, vagal nerve)
- Feasibility of repeat POEM and salvage laparoscopic myotomy if initial POEM fails.
Conversely, POEM (posterior approach) may be a rescue treatment option for unsuccessful laparoscopic myotomy.
POEM also allows for treatment of certain conditions, including diffuse esophageal spasm, that are not amenable to surgical therapy via a laparoscopic approach.
"POEM appears to combine the performance of surgical myotomy with the safety profile of an endoscopic procedure," explains Dr. Wong Kee Song. "Although the published studies have some limitations, available data show that the procedure is effective, at least in the short to intermediate term, in more than 90 percent of achalasia patients."
Multiple systematic reviews and meta-analyses have compared POEM and LHM and showed no significant differences in symptom improvement, and in perioperative outcomes such as procedure time, pain and analgesic use, length of hospital stay and adverse events. POEM is associated with significant decreases in the mean lower esophageal sphincter pressure and integrated relaxation pressure, and improvement on timed barium esophagram.
Several studies show that the incidences of symptomatic GERD after POEM and after LHM with fundoplication are comparable or minimally increased. According to Dr. Fukami, one possible explanation may be related to what POEM does not do. "We're not disrupting the angle of His, so the natural structure that prevents GERD is still present," explains Dr. Fukami. Further technical modifications are underway to reduce the risk of GERD without fundoplication.
According to Timothy A. Woodward, M.D., a therapeutic endoscopist at Mayo Clinic's campus in Florida, certain factors may help predict which patients may not respond as well to POEM. "A study published in Surgical Endoscopy in 2017 showed that a simple assessment of swallowing difficulty, the Eckardt score, seems to predict failure and recurrence," says Dr. Woodward. "This, in turn, may help guide therapeutic approaches."
Dr. Fukami also has praise for the durability of the response to POEM documented thus far. "Data from centers that have performed a large volume of POEM procedures show that the treatment response rate at three months post-procedure is 90 to 100 percent, and the treatment effect decline is 1 percent per year over a three-year period, both of which are similar to results achieved with surgical Heller myotomy."
With the success of POEM in the treatment of achalasia, other esophageal disorders have been treated successfully with this procedure. "The literature, as well as our small series, demonstrate feasibility and efficacy in the treatment of select motility disorders such as jackhammer and spastic esophagus," explains Dr. Woodward.
Challenges
Mayo endoscopists who perform POEM acknowledge that this is a technically challenging procedure, with a steep learning curve, so it should be performed by endoscopists with advanced skills in high-volume centers of excellence.
In an article published in 2017 in the European Journal of Cardio-Thoracic Surgery, thoracic surgeons and gastroenterologists at Mayo Clinic's campus in Rochester, Minnesota, addressed the technical challenges involved in training to perform POEM. The article introduces a novel approach to initiating a POEM program as a helpful bridge for endoscopists and medical centers interested in starting a similar program.
Summary
POEM has shown a steady success rate and promising outcomes since its introduction in 2010. Because of its efficacy and safety profile, the POEM procedure is here to stay, and it is a welcome addition to the armamentarium of treatments available for achalasia and other selected esophageal motility disorders. The results of large, randomized studies comparing POEM and LHM are awaited.
For more information
Ren Y, et al. Pre-treatment Eckardt score is a simple factor for predicting one-year peroral endoscopic myotomy failure in patients with achalasia. Surgical Endoscopy 2017;31:3234.
Reinersman JM, et al. A novel strategy to initiate a peroral endoscopic myotomy program. European Journal of Cardio-Thoracic Surgery. 2017;52:686.