April 13, 2018
Elizabeth Rajan, M.D., a gastroenterologist and therapeutic endoscopist at Mayo Clinic's campus in Rochester, Minnesota, answers several questions about the role of endoscopic full-thickness resection (EFTR) and endoscopic full-thickness biopsy (EFTB) in the management of epithelial and subepithelial lesions and diagnosis of neuromuscular disorders such as gastroparesis.
What challenges does clip-assisted EFTR help address?
Standard polypectomy, endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are established techniques for the resection of superficial neoplasms involving the mucosa and submucosa of the GI tract. EFTR techniques are evolving as an alternative for the removal of lesions that are not amenable to conventional resection techniques. These include:
- Small subepithelial lesions (SELs) arising from the muscularis propria (MP)
- Select non-lifting epithelial lesions associated with fibrosis
- Scarring and lesions in locations that are difficult to access or at high-risk of adverse events, such as within a diverticulum
Although endoscopic resection of SELs involving the MP was previously considered a contraindication owing to a high perforation rate, EFTR offers a safe and effective method to capture the entire GI wall, including the MP. Refinement in resection tools and closure devices and increased experience with EFTR techniques have minimized this adverse event.
Does clip-assisted EFTR always involve all layers of the gastrointestinal (GI) wall?
Yes.
Can you describe the clip-assisted EFTR technique?
Clip-assisted endoscopic full-thickness resection of a subepithelial lesion
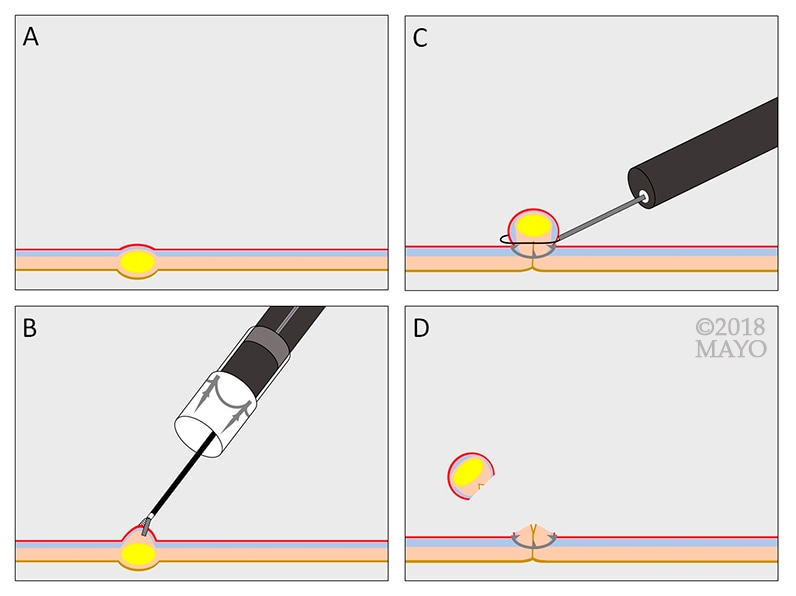
Clip-assisted endoscopic full-thickness resection of a subepithelial lesion
Clip-assisted endoscopic full-thickness resection of a subepithelial lesion. A. Gastrointestinal stromal tumor (GIST) located in the muscularis propria. B. Retraction of the GIST into the cap of an over-the-scope (OTS) clip, followed by clip deployment. C. Resection of the full-thickness pseudopolyp above the clip using hot snare. D. Effective closure of the resection site.
Over-the-scope (OTS) clip-assisted EFTR is emerging as a new, potentially safer alternative that involves securing the defect before providing full-thickness resection of lesions ('close then cut'), avoiding overt perforation and contamination of the peritoneal cavity. This technique may be considered for select non-lifting epithelial lesions such as adenoma that are associated with severe fibrosis from prior resection attempts, and small SELs, including neuroendocrine tumors and gastrointestinal stromal tumors (GISTs). In general, OTS clip-assisted EFTR is suitable for lesions that are < 1 cm in the upper GI tract and < 2 cm in the colorectum. Additional study is needed to examine the use of OTS clip-assisted EFTR for early T1 cancers and lesions > 2 cm in size.
What is the role of endoscopic full-thickness biopsy (EFTB) in diagnosis?
EFTB may enhance our understanding of the pathophysiology and guide therapy for gastrointestinal neuromuscular diseases, as well as other inflammatory and neoplastic conditions. By facilitating the acquisition of the intermuscular layer of the MP, EFTB allows for evaluation of the networks of myenteric plexus and interstitial cells of Cajal (ICC) that lie within this layer.
Because it's thought that some disorders are associated with an underlying heterogeneous neuromuscular pathology, EFTB may thus advance our understanding of the etiology and potential therapy for GI disorders whose pathophysiology is largely unknown, such as functional dyspepsia, idiopathic gastroparesis and chronic intestinal pseudo-obstruction. Because it can provide access to large tissue specimens, EFTB may also offer important diagnostic advantages over endoscopic ultrasound (EUS)-guided fine-needle aspiration or biopsy for some lesions.
What do available research data show us about the safety and efficacy of EFTR and EFTB?
Results published thus far are promising, but prospective comparative studies are needed to assess long-term efficacy and safety of these techniques. For more information about available safety and efficacy data, please see our team's article in Gastroenterology.
Who should perform these procedures?
EFTR and EFTB should be performed by appropriately trained advanced therapeutic endoscopists. Similar to other invasive procedures, no standardized protocol for training and assessment of competence is currently available. In experienced hands, EFTR represents a viable option for the removal of select lesions in the least invasive fashion. Future societal guidelines will be instrumental in directing training.
For more information
Rajan E, et al. Endoscopic full thickness resection. Gastroenterology. In press.