Nov. 11, 2025
The jaw has a complex anatomy and an essential function. Tumors that occur in the mandible often require the removal of a large portion of bone. Highly specialized mandible reconstruction techniques enable patients to maintain their appearance while also preserving their ability to chew and swallow.
One important technique in reconstruction is the use of vascularized tissue free flaps, typically from the fibula or iliac crest. "As little as a decade ago, surgeons would measure and fit flaps by hand, which lacked precision and accuracy," says Kyle S. Ettinger, M.D., D.D.S., an oral and maxillofacial surgeon and surgical oncologist at Mayo Clinic in Rochester, Minnesota. "Today, image-generated computer models and 3D-printed cutting guides and plating trays give us millimeter precision in performing reconstructions unique to the patient's anatomy. Microvascular surgery tools and surgical optics have also improved over the decades, allowing us to reliably connect small blood vessels with nylon thread thinner than a human hair."
Dr. Ettinger describes mandibular resection and reconstruction in a 58-year-old patient with ameloblastoma, a rare tumor that starts in tooth-forming cells. While almost always benign, ameloblastoma can be locally invasive and recur after treatment. In extremely rare cases, it can become cancerous and spread to other areas of the body.
Selecting the most effective treatment
Ameloblastoma is usually asymptomatic. Dentists may detect tumors on routine X-rays or when patients seek care for swelling that happens as tumors grow large.
"This patient in this case study came to Mayo Clinic in 2016 via referral from an oral surgeon after seeing a dentist for pain, which is not a typical presentation," says Dr. Ettinger. Panoramic X-rays and a biopsy confirmed a 3-cm ameloblastoma in the canine-premolar region of the right mandible.
Determining the most appropriate surgical approach depends on the type of ameloblastoma and patient factors. Enucleation and curettage are a less aggressive option for unicystic ameloblastomas, which look and behave more like cysts. However, solid subtype ameloblastomas act more like tumors and are more likely to recur after less aggressive treatment. "Because this patient's ameloblastoma was a solid tumor, the recommended approach was to perform resection and reconstruction," says Dr. Ettinger.
Presurgical planning
X-ray and virtual models
X-ray and virtual models
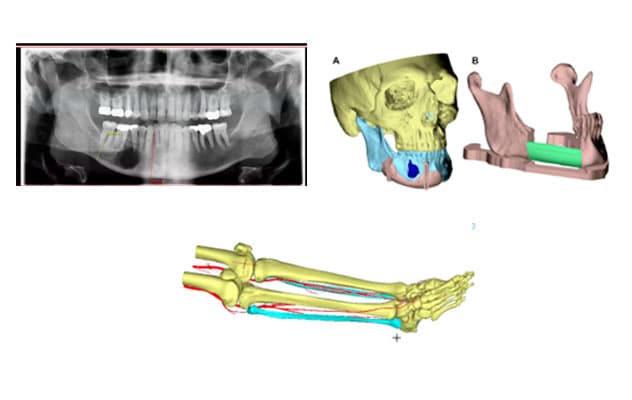
The images show a panoramic X-ray of an ameloblastoma tumor in the lower right mandible; virtual models of the resection planes around the tumor (A) and the area of fibula free-flap insertion (B); and leg detailing fibula anatomy and blood vessel location.
The first step of planning surgery was CT imaging of the head, face and area from which the free flap would be taken — in this case, the fibula. CT angiography of the leg also ensured the patient had the appropriate blood vessel anatomy to allow for fibula free flap harvest, since the procedure requires removing one of the three main arteries to the foot for use in the reconstruction.
"We worked with biomedical engineers in Mayo Clinic's 3D Anatomic Modeling Laboratories to load the CT images into the software and convert them into 3D virtual models in a process called segmentation," says Dr. Ettinger. "The software can color-code the different anatomical structures and produce images that the surgeon can virtually move and view from any angle."
Dr. Ettinger used the software to establish the virtual cutting planes with 1-centimeter margins around the tumor. He also planned the reconstruction based on fibula architecture and blood vessel location.
Resection and reconstruction
A large team of professionals, including surgeons, anesthesiologists, surgical technologists and nurses, participated in this complex surgery. Two maxillofacial surgeons, both trained in tumor resection and microvascular reconstruction, performed the surgery. Working in tandem allows the surgery to be performed efficiently and can help reduce the length of surgery, which improves patient outcomes.
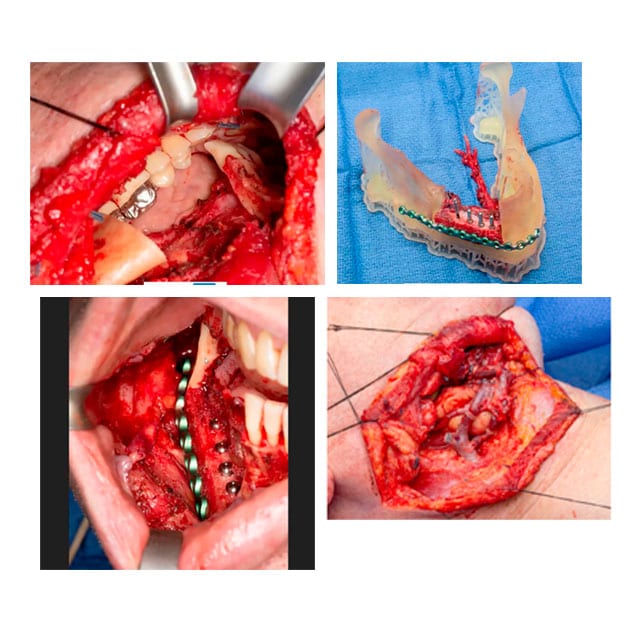
During the reconstruction, one surgeon removed the tumor and identified blood vessels in the neck to connect to the free flap. The other removed and prepared the fibular free flap. In the operating room, a 3D-printed plating tray was used to preassemble the:
- Fibula free flap.
- Titanium plate attaching the flap to the jawbone.
- Implants for the prosthetic dental reconstruction.
Dr. Ettinger also reconstructed the sensory nerve in the lower jaw with a cadaver nerve graft. Because this sensory nerve runs through the mandible, it was removed along with the tumor. Nerve reconstruction enabled the patient to regain sensation in the lip and the chin during the recovery process.
Although this patient didn't need a temporary tracheostomy due to the tumor's location and size, some patients require one during surgery. A tracheostomy helps ensure the patient's airway is protected and breathing can occur safely during and after surgery.
Reestablishing blood flow to the free flap
 Free-flap reconstruction
Free-flap reconstruction
The images show a resected area prior to reconstruction, a preassembly tray with fibula free flap, titanium plate and implants. The completed free-flap reconstruction and nerve graft and neck access show completed microvascular connection.
Survival of the free flap depends on connecting the blood vessels and keeping them open and flowing. Using a surgical microscope, Dr. Ettinger connected the blood vessels in the flap to those in the neck, allowing blood to flow into the flap via the arteries and out of the flap via the veins. From start to finish, these surgeries typically take about 4 to 6 hours.
Postsurgery care
Patients spend a minimum of five days in the hospital under the close care of a specialized nursing team. "Prior studies have shown that most clotting and bleeding issues happen within the first five days after free-flap surgery; therefore, patients stay in the hospital until this window of concern has passed," says Dr. Ettinger. "To monitor blood flow in the newly connected blood vessels, we relied on an implanted Doppler device placed during surgery. The patient also had a feeding tube to assist with nutrition and hydration after surgery."
The first follow-up visit was one week after discharge. Dr. Ettinger encourages patients who live out of town to stay in the area during that time. "Being close by allows us to rapidly and appropriately treat any problems that arise," he says.
Additional follow-up for this patient included three months of healing followed by a second minor surgical procedure to uncover the implants placed during the initial surgery. This period allowed maxillofacial prosthodontists to begin making the prosthetic replacement teeth. "We work closely with the prosthodontists to ensure patients have a balanced, esthetic and functional dental prosthetic reconstruction after surgeries such as these," says Dr. Ettinger.
 Final appearance
Final appearance
Image shows the final appearance with the prosthetic dental bridge in place.
The final dental prosthesis was inserted one month later. Nine years later, the patient is doing well and has had no tumor recurrence.
Dr. Ettinger completes 60 to 70 free-flap surgeries a year with a success rate of 96% to 98%. "We optimize all aspects of care within our control to provide the best possible outcome for patients," he says.
For more information
Ettinger KS, et al. Mandibular reconstruction: When to graft, when to flap and when to say no. Atlas of the Oral & Maxillofacial Surgery Clinics of North America. 2023;31:91.
Refer a patient to Mayo Clinic.