Colon cancer is one of the most common cancers worldwide. Early detection can dramatically improve outcomes. One of the simplest ways you can monitor your digestive health is by paying close attention to changes in your stools. Not all stool changes mean you have cancer, but some are important to tell a healthcare professional about.
Why does colon cancer affect stool appearance?
The colon's main job is to process digested food, absorb water and form stools, which are then removed from the body. When cancer grows in the colon, it can block or change the way stool moves through the intestines. Cancer also can cause bleeding or interfere with the absorption of nutrients and water. When this happens, you might see changes in how the stool looks or the size or how often you go to the bathroom.
What signs should you look for in your stool?
Heces del cáncer de colon
Heces del cáncer de colon
No todos los cambios en las heces significan que tienes cáncer, pero algunos pueden ser señales de alerta. Cuando se desarrolla cáncer en el colon, puede afectar el aspecto y el tamaño de las heces, además de la frecuencia con la que vas al baño.
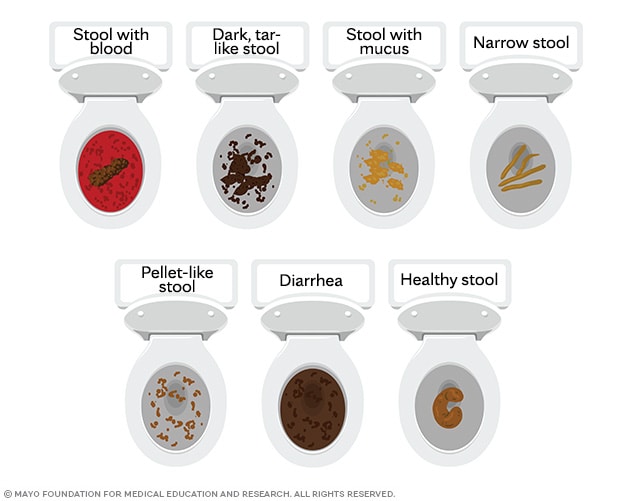
Even though early colon cancer might not cause any signs, here are some stool changes that could be warning signs:
- Blood in your stool. You might see bright red blood or very dark, black, tarlike stool. Blood from lower down in your colon or rectum is usually red. Bleeding from higher up in the colon can make stools look black.
- Skinny or thin stool. A sudden change to ribbon-thin or pencil-thin stool might happen if cancer is making the passage smaller.
- Change in how often you have a stool. If you have diarrhea or constipation that lasts more than a few days, talk with a healthcare professional.
- Mucus in stool. Stool often contains a small amount of mucus. Mucus is a jellylike substance that your intestines make to keep the lining of your colon moist and lubricated. But you should talk to a healthcare professional if you notice an increased amount of mucus in stool.
How stools may change with different stages of colon cancer
Stage 0 and stage 1 colon cancer
In the early stages of colon cancer, the cancer is smaller and hasn't spread outside the colon. Most people likely won't notice any difference in their stools. There may be a small bit of blood in the stool that's hard to see.
Stage 2 colon cancer
In stage 2, the colon cancer has spread into the outermost layers of the colon and possibly nearby tissues or organs. You may notice:
- Visible blood in your stools.
- Stools that start to look thinner.
- Going to the bathroom more often or feeling like you can't finish.
Stage 3 colon cancer
In stage 3, the colon cancer has grown bigger and has spread into nearby lymph nodes. You may notice:
- Pencil-thin stools happen more often.
- Diarrhea or constipation won't go away.
- More blood and mucus in the stools.
Stage 4 colon cancer
In stage 4, colon cancer has spread to other parts of the body. This is called metastatic or distant colon cancer. At this stage, the colon might be blocked or not function well. You may notice:
- Stools may be very thin or may look like pellets. Or you might not be able to pass stools at all.
- Blood in stools is common, and stools can be very dark.
- Severe stomach pain and swelling.
Other conditions that can look like colon cancer
A few other conditions can affect your stools, including:
- Swollen veins in the anus and lower rectum, called hemorrhoids.
- A small tear in the thin, moist tissue that lines the anus, called an anal fissure.
- Inflammatory bowel diseases, such as Crohn's disease or ulcerative colitis.
- Infection.
- Certain foods or medicines.
When should you see a doctor?
See a healthcare professional if you notice:
- Red or black stool color, which could mean bleeding.
- Stools that stay thin, ribbonlike or pencil-shaped for more than a few days.
- Diarrhea or constipation for more than a few days.
- Stomach pain you can't explain.
- Feeling like you can't finish passing stool.
- Feeling unwell without any obvious reason.
What are your screening options?
Health professionals recommend everyone starts screening for colon cancer at age 45, or earlier for those with a family history of colon cancer. Colonoscopy is the most widely used and most accurate screening test for colorectal cancer in the U.S., but it is invasive and requires sedation. Less invasive, at-home test kits are available. While more convenient and affordable, these tests are less accurate than colonoscopy and still require follow-up with colonoscopy if results are positive.
At-home stool tests
There are easy-to-use stool tests you can do at home to help find colon cancer. These tests check stools for blood or changes in DNA. They work best for finding cancers that are more advanced, but they also can sometimes find early cancers.
At-home tests can't tell you the stage of the cancer. Stool tests are for detection only. Staging requires imaging and biopsy. The right test for you depends on your age and risk. Be certain to ask your healthcare team which of these options is best for your particular situation.
Available at-home tests include:
- Fecal occult blood tests (FOBTs). These tests should be done once a year for people at average risk. A positive result should always be followed by colonoscopy. There are two types of FOBTs:
- Fecal immunochemical test (FIT). FIT uses antibodies to detect blood in the stool and offers better accuracy than guaiac-based FOBT (gFOBT). The text is simple. It requires no special diet preparation and has been shown to reduce colon cancer mortality in large studies. After a positive FIT, colonoscopy is needed. If colonoscopy results are typical and you have no symptoms, you can return to screening every 10 years.
- Guaiac-based FOBT (gFOBT). This test detects blood using a chemical reaction but has lower sensitivity than other tests. It requires a special diet beforehand and is less likely to detect early cancers or polyps. Participation and detection rates are lower than with FIT, making it a less favored option.
- Multitarget stool DNA test (mt-sDNA). The mt-sDNA test checks for both hidden blood and specific DNA changes linked to colon cancer. This test is better than FIT at detecting cancer and advanced precancerous growths. However, it may produce more false positives. This test is approved for average-risk adults age 45 and older and is recommended every 1 to 3 years. If colonoscopy after a positive mt-sDNA test is negative and you have no symptoms, you can return to regular screening every 10 years. One stool DNA test (Cologuard) is approved for colon cancer screening in the United States.
- Multitarget stool RNA test (mt-sRNA). The mt-sRNA test is a newer option that detects RNA markers and blood. It also considers smoking status. It's more sensitive than FIT for both cancer and advanced polyps. Like the mt-sDNA test, the mt-sRNA test may produce more false positives than FIT. This test is approved for average-risk adults age 45 and older and is recommended every three years. Like other stool tests, a positive result should be followed by colonoscopy. If colonoscopy after a positive mt-sRNA test is negative and you have no symptoms, you can return to regular screening every 10 years.
Sept. 09, 2025
- Colorectal cancer. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/colorectal-cancer. Accessed Aug. 4, 2025.
- Colon cancer treatment (PDQ) — Patient version. National Cancer Institute. https://www.cancer.gov/types/colorectal/patient/colon-treatment-pdq. Accessed Aug. 4, 2025.
- Elsevier Point of Care. Clinical Overview: Colorectal cancer. https://www.clinicalkey.com. Accessed Aug. 4, 2025.
- Colon cancer. National Comprehensive Cancer Network guidelines for patients. https://www.nccn.org/guidelines/category_1. Accessed Aug. 4, 2025.
- Colorectal cancer symptoms: 7 signs to know. Fight Colorectal Cancer. https://fightcolorectalcancer.org/facts/symptoms/. Accessed Aug. 4, 2025.
- Ferri FF. Colon cancer. In: Ferri's Clinical Advisor 2026. Elsevier; 2026. https://www.clinicalkey.com. Accessed July 22, 2025.
- Colorectal cancer screening. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1429. Accessed July 22, 2025.
- Bowel cancer symptoms: Your questions answered. Bowel Cancer UK. https://www.bowelcanceruk.org.uk/news-and-blogs/research-blog/bowel-cancer-symptoms-your-questions-answered/. Accessed Aug. 4, 2025.
- Han F, et al. Clinicopathological features and prognosis analysis of proximal colonic mucinous adenocarcinoma. Scientific Reports. 2024; doi:10.1038/s41598-024-69916-0.
- Herath M, et al. The role of the gastrointestinal mucus system in intestinal homeostasis: Implications for neurological disorders. Frontiers in Cellular and Infection Microbiology. 2020; doi:10.3389/fcimb.2020.00248.
- Medical review (expert opinion). Mayo Clinic. Aug. 5, 2025.