Overview
Sleep apnea is a potentially serious condition that causes breathing to stop and start several times during sleep. People with the condition snore loudly and feel tired even after a full night of sleep.
The main types of sleep apnea are:
- Obstructive sleep apnea. Also known as OSA, this more common form of sleep apnea occurs when throat narrowing blocks the flow of air into the lungs.
- Central sleep apnea. Also known as CSA, this type of sleep apnea occurs when the brain doesn't send proper signals to the muscles that manage breathing.
- Treatment-emergent central apnea syndrome, also known as complex sleep apnea. This form of sleep apnea happens when OSA — diagnosed with a sleep study — converts to CSA when receiving sleep apnea therapy.
Sleep apnea treatment can ease symptoms and might help prevent complications, such as heart problems.
Products & Services
Symptoms
The symptoms of obstructive sleep apnea and central sleep apnea overlap. Sometimes it's hard to know which type you have. The most common symptoms include:
- Loud snoring.
- Episodes in which breathing stops during sleep, which would be reported by another person.
- Gasping for air during sleep.
- Awakening with a dry mouth.
- Morning headaches.
- Trouble staying asleep, known as insomnia.
- Excessive daytime sleepiness, known as hypersomnia.
- Trouble paying attention while awake.
- Irritability.
When to see a doctor
Loud snoring can indicate a potentially serious problem, but not everyone who has sleep apnea snores. Talk to your healthcare professional if you have symptoms of sleep apnea or any sleep problem that leaves you very tired, sleepy and irritable.
Causes
Obstructive sleep apnea
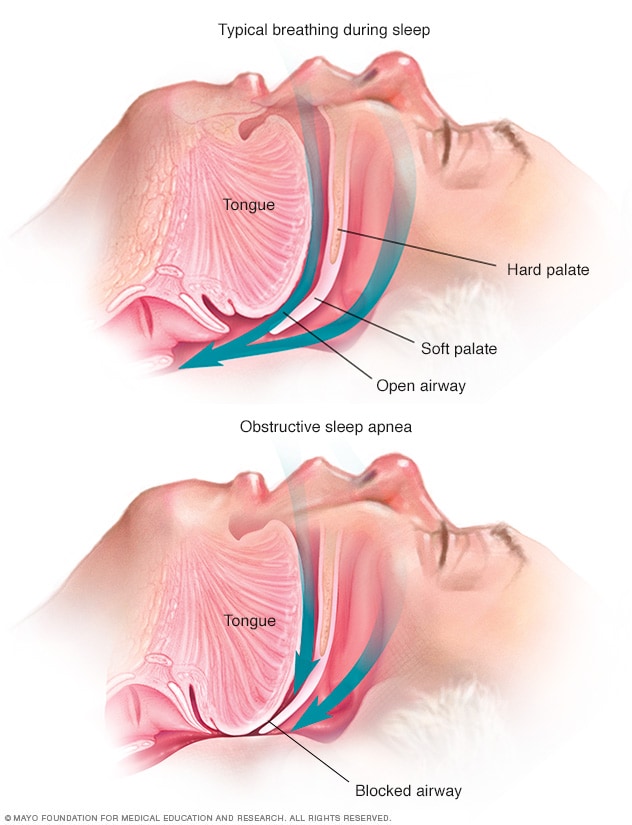
Obstructive sleep apnea
Obstructive sleep apnea occurs when the muscles that support the soft tissues in your throat, such as your tongue and soft palate, relax briefly. When these muscles relax, your airway is narrowed or closed, and breathing is momentarily cut off.
Obstructive sleep apnea and central sleep apnea have different causes.
Obstructive sleep apnea
This type of sleep apnea happens when the muscles in the back of the throat relax. These muscles support the back of the roof of the mouth, known as the soft palate. The muscles also support the tongue, tonsils, side walls of the throat, and the tissue hanging from the soft palate, called the uvula.
When the muscles relax, your airway narrows or closes as you breathe in. You can't get enough air, which can lower the oxygen level in your blood. Your brain senses your inability to breathe and briefly wakes you so that you can reopen your airway. This awakening is usually so brief that you don't remember it.
You might snort, choke or gasp. This pattern can repeat itself 5 to 30 times or more each hour, all night, affecting your ability to reach the deep, restful phases of sleep.
Central sleep apnea
This less common form of sleep apnea occurs when your brain fails to send signals to your breathing muscles. This means that you make no effort to breathe for a short period. You might awaken with shortness of breath or have a hard time getting to sleep or staying asleep.
Risk factors
Sleep apnea can affect anyone, even children, but certain factors raise your risk.
Obstructive sleep apnea
Factors that increase the risk of this form of sleep apnea, also known as OSA, include:
- Excess weight. Obesity greatly increases the risk of OSA. Fat deposits can block your upper airway and affect your breathing.
- A narrowed airway. You might have inherited a narrow throat. Tonsils or adenoids also can enlarge and block the airway, particularly in children. People with thicker necks also might have narrower airways.
- Sex assigned at birth. Men are 2 to 3 times more likely to have sleep apnea than are women. However, women's risk is increased if they're overweight or if they've gone through menopause.
- Being older. OSA is more common in older adults.
- Family history. Having family members with OSA might increase your risk.
- Use of alcohol or sedatives. These substances relax the muscles in your throat, which can worsen OSA.
- Smoking. Smokers are three times more likely to have OSA than are people who've never smoked. Smoking can increase the amount of inflammation and fluid retention in the upper airway.
- Nasal congestion. If you have trouble breathing through your nose, you're more likely to start to get OSA. This can be due to your anatomy or allergies.
- Medical conditions. Congestive heart failure, high blood pressure and type 2 diabetes are some of the conditions that may increase the risk of OSA. Polycystic ovary syndrome, hormonal disorders and prior stroke also may raise the risk.
Central sleep apnea
Risk factors for this form of sleep apnea, also known as CSA, include:
- Being older. Middle-aged and older people have a higher risk of CSA.
- Sex assigned at birth. CSA is more common in men than it is in women.
- Heart disorders. Having congestive heart failure increases the risk.
- Using opioid medicines. Opioid medicines, especially long-acting ones such as methadone, increase the risk of CSA.
- Stroke. Having had a stroke increases your risk of CSA.
Complications
Sleep apnea is a serious medical condition. Complications of obstructive sleep apnea, also known as OSA, can include:
-
Feeling very tired during the day. The repeated awakenings caused by sleep apnea make typical, restorative sleep impossible. In turn, OSA causes severe daytime drowsiness and irritability.
You might not be able to concentrate or find yourself falling asleep at work, while watching TV or even when driving. People with OSA have an increased risk of motor vehicle and workplace accidents.
You also might feel quick-tempered, moody or depressed. Children and teenagers with OSA might perform poorly in school or have behavior problems.
-
High blood pressure or heart problems. Sudden drops in blood oxygen levels that occur during OSA increase blood pressure and strain the cardiovascular system. Having OSA increases your risk of high blood pressure, also known as hypertension.
OSA also might increase your risk of recurrent heart attack, stroke and irregular heartbeats, such as atrial fibrillation. If you have heart disease, multiple episodes of low blood oxygen can lead to sudden death from an irregular heartbeat.
- Type 2 diabetes. Having OSA increases your risk of getting insulin resistance and type 2 diabetes.
- Metabolic syndrome. People with OSA can have this syndrome, which includes having hypertension, elevated cholesterol levels, high blood sugar and an increased waist circumference. This syndrome is linked to a higher risk of heart disease.
- Complications with medicines and surgery. OSA is also a concern with certain medicines and general anesthesia. People with OSA might be more likely to have complications after major surgery because they're prone to breathing problems, especially when sedated and lying on their backs. Before surgery, it's important to tell your healthcare professional about your OSA and how it's treated.
- Liver problems. People with OSA are more likely to have irregular results on liver function tests. Their livers also are more likely to show signs of scarring, known as nonalcoholic fatty liver disease.
- Sleep-deprived partners. Loud snoring can keep anyone who sleeps nearby from getting good rest. Sometimes a partner has to go to another room, or even on another floor of the house, to sleep.
Complications of central sleep apnea, also known as CSA, can include:
- Feeling very tired. CSA causes repeated awakenings, making it very hard to get restful sleep. People with CSA often have daytime drowsiness and irritability. It interferes with concentration and can cause people to fall asleep at work, while watching television or even while driving.
- Cardiovascular problems. Sudden drops in blood oxygen levels that occur during CSA can affect heart health. If there's underlying heart disease, repeated episodes of low blood oxygen increase the risk of irregular heart rhythms.
Prevention
Sleep apnea may not be able to be prevented in everyone, but addressing risk factors can decrease the likelihood of breathing problems during sleep. To decrease OSA risk, healthcare professionals recommend losing excess weight, treating nasal congestion and not drinking more than a moderate amount of alcohol. To lower CSA risk, minimize your use of opioid medicines and see your healthcare professional if you have congestive heart failure.
Dec. 09, 2025