Diagnosis
Female cystoscopy
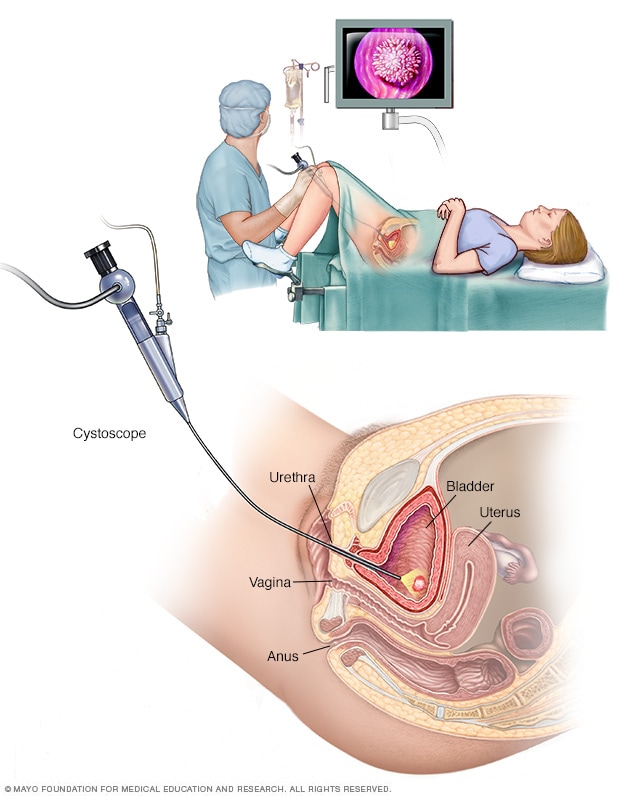
Female cystoscopy
Cystoscopy uses a thin, flexible tool with a light on the end, called a cystoscope. This allows a healthcare professional to see the inside of the urethra and bladder to diagnose conditions that affect the urinary tract.
Male cystoscopy
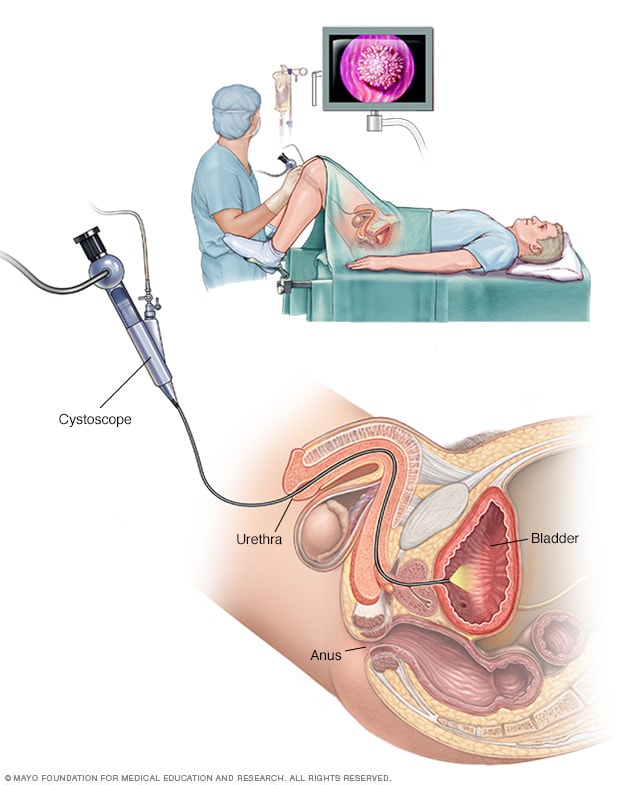
Male cystoscopy
Cystoscopy uses a thin, flexible tool with a light on the end, called a cystoscope. This allows a healthcare professional to see the inside of the urethra and bladder to diagnose conditions that affect the urinary tract.
Tests and procedures used to diagnose urinary tract infections include:
- Analyzing a urine sample. You may be asked for a urine sample. A lab can check the urine for white blood cells, red blood cells or bacteria. You may need to first wipe your genital area with an antiseptic pad and then collect the urine midstream, a second or two after you start passing urine into the toilet. This helps prevent the sample from being contaminated.
- Growing urinary tract bacteria in a lab. Lab analysis of urine is sometimes followed by a urine culture. This test checks what bacteria are causing the infection. The culture results help your healthcare professional know what medicines will be most effective in treating your condition.
- Creating images of the urinary tract. UTIs that come back, called recurrent UTIs, may happen because of problems with the structures in the urinary tract. Imaging tests, such as ultrasound, CT scan or MRI, show the structures in the urinary tract. The images may help your healthcare team see what's causing the UTIs.
- Using a scope to see inside the bladder. For recurrent UTIs, your healthcare professional may talk with you about an exam called cystoscopy. The exam uses a long, thin tube with a lens, called a cystoscope, to see inside the urethra and bladder.
Treatment
Antibiotics often are the first treatment for an active urinary tract infection. Your health and the type of bacteria in your urine guide which medicine is used and how long you need to take it.
Simple infections
Antibiotics used to treat simple UTIs include:
- Trimethoprim and sulfamethoxazole (Bactrim, Bactrim DS).
- Fosfomycin.
- Nitrofurantoin (Macrodantin, Macrobid, Furadantin).
- Cephalexin.
- Ceftriaxone.
Fluoroquinolones aren't used for most simple UTIs. This group of antibiotics includes ciprofloxacin (Cipro), levofloxacin and others. Their risks tend to outweigh the benefits for simple UTIs. But for complicated UTIs or kidney infections, a a fluoroquinolone medicine might be used if there are no other treatment options.
Often, UTI symptoms begin to clear up within a few days of starting treatment. But it may take some time for inflammation to go down and symptoms to get better. Depending on the infection and the specific medicine, you may need to keep taking antibiotics for a week or more. Take all the medicine as instructed.
For a simple UTI that happens when you're otherwise healthy, a healthcare professional may suggest a shorter course of treatment. That may mean taking an antibiotic for 1 to 3 days. Whether a short course of treatment is enough to treat your infection depends on your symptoms, the type of antibiotic and your medical history.
Your healthcare professional also may give you a medicine to lessen burning when you urinate. But pain tends to go away soon after starting an antibiotic.
Preventing repeat infections
After being treated for a urinary tract infection, it's important to think about ways to prevent an infection from happening again. These steps may help lower your risk of future UTIs:
- Drink plenty of fluids, especially water. Drinking water helps dilute the urine. That leads you to urinate more often. Urinating flushes bacteria away before an infection can start. Aim for 1.5 liters, or around 50 ounces, or more of fluids each day, unless your healthcare team tells you to take in a different amount based on other medical conditions.
- Try topical vaginal estrogen therapy. For women who are in perimenopause or menopause, using a product in the vagina that contains estrogen can help reduce the risk of a repeat UTI. Vaginal estrogen therapy is only appropriate if there are no medical reasons why you shouldn't use estrogen therapy.
- Manage constipation. Eat more fruits, vegetables, beans, whole-grain bread and other fiber-rich foods. Regular physical activity also helps improve the movement of stool through the colon.
- Try cranberry juice. Researchers keep studying cranberry juice and other cranberry products to learn whether they might help prevent UTIs. For now, results are unclear. There's little harm in drinking cranberry juice if you feel it helps you prevent UTIs, but watch the calories and sugar in some products. For most people, drinking cranberry juice is safe. Some people report an upset stomach or diarrhea. Don't drink cranberry juice if you're taking blood-thinning medicine, such as warfarin (Jantovin).
- Avoid feminine products that might irritate the skin. Deodorant sprays, douches and powders in the genital area can irritate the urethra.
- Change your birth control method. Diaphragms, condoms that are not lubricated and condoms treated with spermicide can add to bacterial growth.
Your healthcare professional may talk with you about other strategies to keep UTIs from coming back. These strategies may include taking certain supplements or medicines that aren't antibiotics.
Frequent infections despite preventive efforts
Sometimes UTIs keep coming back even with careful use of preventive strategies that don't involve antibiotics. When this happens, your healthcare professional may suggest other ways of using antibiotics, such as:
- Diagnosing and treating yourself when symptoms occur. This is called self-start therapy. You'll be asked to stay in touch with your healthcare professional during self-start therapy.
- Taking a single dose of an antibiotic after sex if your UTIs seem to happen after sexual activity.
- Using low-dose antibiotics for an extended period. You might take them for six months or longer.
Antibiotics can have unwanted side effects, such as a skin rash, upset stomach or loose stools. Overuse of antibiotics also can lead to antibiotic resistance. Antibiotic resistance happens when bacteria become stronger than the drugs designed to kill them. That's why it's important to try to prevent UTIs from coming back with strategies that don't use antibiotics.
Severe infections
For severe UTIs, you may need IV antibiotics given in a hospital.
Lifestyle and home remedies
Urinary tract infections can be painful, but there are some things you can try that may ease discomfort until the antibiotics take effect. For example:
- Drink plenty of water. Water helps to dilute urine and flush out bacteria.
- Avoid drinks that may bother your bladder. Avoid coffee, alcohol, and soft drinks that have citrus juices or caffeine until the infection clears. They can irritate the bladder and add to the need to urinate.
- Use a heating pad. Put a warm, but not hot, heating pad on your belly. This can help lessen bladder pressure or discomfort.
Preparing for your appointment
A primary care doctor, nurse practitioner or other healthcare professional can treat most UTIs. If you have frequent UTIs or a chronic kidney infection, you may see a doctor who specializes in urinary conditions, called a urologist or urogynecologist. Or you may see a doctor who specializes in kidney conditions, called a nephrologist.
What you can do
To get ready for your appointment:
- Ask if there are things you need to do in advance, such as collect a urine sample.
- Take note of your symptoms, even if you're not sure they're related to a UTI.
- Make a list of all the medicines, vitamins or other supplements that you take.
- Write down questions to ask your healthcare team.
For a UTI, basic questions to ask include:
- What's the most likely cause of my symptoms?
- Are there any other possible causes?
- Do I need any tests to confirm the diagnosis?
- What factors do you think may have contributed to my UTI?
- What treatment approach do you think is best for me?
- If the first treatment doesn't work, what will you advise next?
- Am I at risk of complications from this condition?
- What is the risk that the UTI will come back?
- What steps can I take to lessen the risk of it coming back?
- Should I see a specialist?
Be sure to ask any other questions that come to mind during the appointment.
What to expect from your doctor
Questions that your doctor or other healthcare professional might ask include:
- When did you first notice your symptoms?
- Have you ever been treated for a bladder or kidney infection?
- How severe is your discomfort?
- How often do you urinate?
- Does urinating relieve your symptoms?
- Do you have low back pain?
- Have you had a fever?
- Have you noticed vaginal discharge or blood in your urine?
- Are you sexually active?
- Do you use birth control? What kind?
- Could you be pregnant?
- Are you being treated for any other medical conditions?
- Have you ever used a catheter?
Sept. 26, 2025