Overview
Vision with macular degeneration
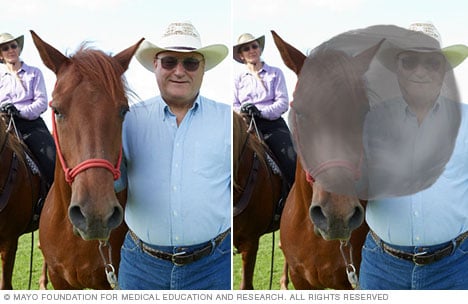
Vision with macular degeneration
As macular degeneration develops, clear, typical vision (left) becomes hazy. With advanced macular degeneration, a blind spot typically forms at the center of the visual field (right).
Dry macular degeneration is an eye condition that causes blurred vision or reduced central vision. It is caused by the breakdown of a part of the retina known as the macula (MAK-u-luh). The macula is responsible for central vision. This condition is common among people over 50.
Dry macular degeneration may start in one eye then develop in the other eye. It also may develop in both eyes at the same time. Over time, vision may worsen and affect the ability to do things, such as read, drive and recognize faces. But having dry macular degeneration doesn't mean you'll lose all your sight. Vision loss is typically central, and people retain their side vision. Some people have only mild central vision loss. In others, it can be more severe.
Early detection and self-care measures may delay vision loss caused by dry macular degeneration.
Mayo Clinic Health Letter & Books
Join thousands of readers who trust Mayo Clinic Health Letter for reliable health tips and insights. Start your journey to better health today.
Products & Services
Symptoms
Dry macular degeneration symptoms usually develop gradually and without pain. They may include:
- Visual distortions, such as straight lines seeming bent.
- Reduced central vision in one or both eyes.
- The need for brighter light when reading or doing close-up work.
- Increased difficulty adapting to low light levels, such as when entering a dimly lit restaurant or theater.
- Increased blurriness of printed words.
- Difficulty recognizing faces.
- A well-defined blurry spot or blind spot in the field of vision.
Dry macular degeneration can affect one or both eyes. If only one eye is affected, you may not notice any changes in your vision. This is because your good eye may compensate for the affected eye. And the condition doesn't affect the side vision, so it does not cause total blindness.
Dry macular degeneration is one of two types of age-related macular degeneration. It can progress to wet macular degeneration, which is when blood vessels grow and leak under the retina. The dry type is more common, but it usually progresses slowly over years. The wet type is more likely to cause a relatively sudden change in vision resulting in serious vision loss.
When to see a doctor
See your eye care professional if:
- You notice changes, such as distortion or blind spots, in your central vision.
- You lose the ability to see fine detail.
These changes may be the first sign of macular degeneration, particularly if you're over age 60.
Causes
Parts of the eye
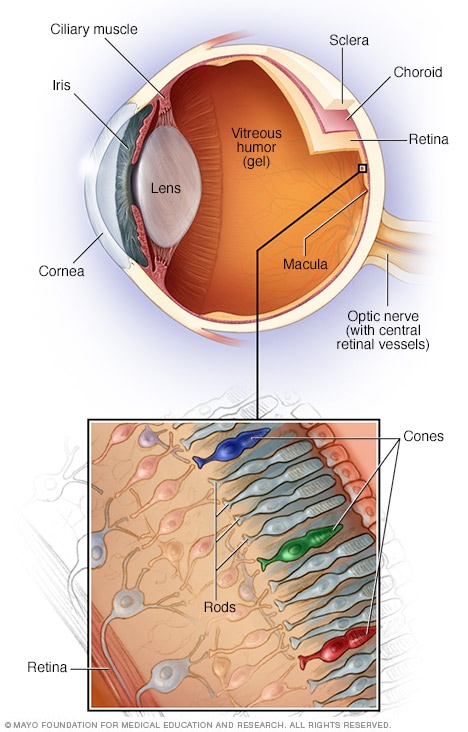
Parts of the eye
The macula is located at the back of the eye in the center of the retina. A healthy macula allows for clear central vision. The macula is made up of densely packed light-sensitive cells called cones and rods. Cones give the eye color vision, and rods let the eye see shades of gray.
No one knows exactly what causes dry macular degeneration. Research suggests that it may be a combination of genes and other factors, including smoking, obesity and diet.
The condition develops as the eye ages. Dry macular degeneration affects the macula. The macula is the area of the retina that's responsible for clear vision in the direct line of sight. Over time, tissue in the macula may thin and lose cells responsible for vision.
Risk factors
Factors that may increase the risk of macular degeneration include:
- Age. This disease is most common in people over 50.
- Family history and genetics. This disease has a hereditary component, meaning it runs in families. Researchers have identified several genes linked to the condition.
- Race. Macular degeneration is more common in white people.
- Smoking. Smoking cigarettes or being exposed to tobacco smoke on a regular basis greatly increases the risk of macular degeneration.
- Obesity. Research suggests that obesity may increase the chance that early or intermediate macular degeneration will progress to the more serious form of the disease.
- Cardiovascular disease. If you have heart or blood vessel disease, called cardiovascular disease, you may be at higher risk of macular degeneration.
Complications
People whose dry macular degeneration has progressed to central vision loss have a higher risk of depression and social isolation. With profound loss of vision, people may see visual hallucinations. This condition is called Charles Bonnet syndrome. Dry macular degeneration may progress to wet macular degeneration, which can quickly cause complete vision loss if left untreated.
Prevention
It's important to have routine eye exams to identify early signs of macular degeneration. The following measures may help reduce the risk of developing dry macular degeneration:
- Manage all medical conditions. For example, if you have cardiovascular disease or high blood pressure, take your medicine and follow your healthcare team's instructions for controlling the condition.
- Don't smoke. People who smoke are more likely to develop macular degeneration than are people who don't smoke. Ask a healthcare professional for help stopping smoking.
- Maintain a healthy weight and exercise regularly. If you need to lose weight, reduce the number of calories you eat and increase the amount of exercise you get each day.
- Choose a diet rich in fruits and vegetables. These foods contain antioxidant vitamins that reduce your risk of developing macular degeneration.
- Include fish in your diet. Omega-3 fatty acids, which are found in fish, may reduce the risk of macular degeneration. Nuts such as walnuts also contain omega-3 fatty acids.
Dec. 06, 2024