Diagnosis
Bone marrow exam
Bone marrow exam
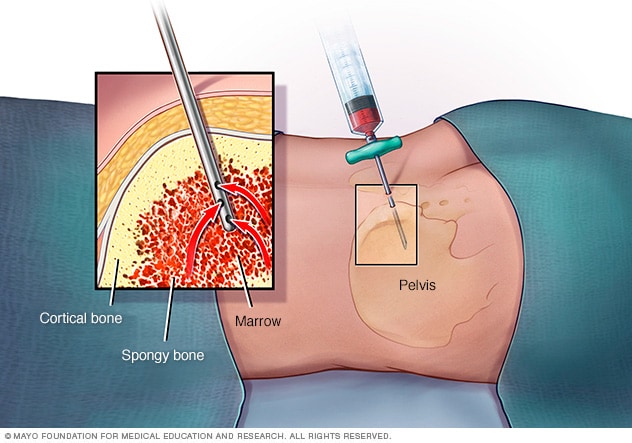
In a bone marrow aspiration, a healthcare professional uses a thin needle to remove a small amount of liquid bone marrow. It is usually taken from a spot in the back of the hip bone, also called the pelvis. A bone marrow biopsy is often done at the same time. This second procedure removes a small piece of bone tissue and the enclosed marrow.
Lumbar puncture, also known as a spinal tap
Lumbar puncture, also known as a spinal tap
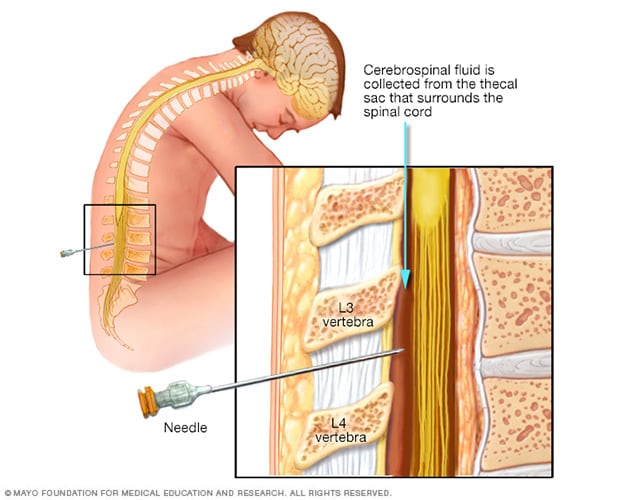
During a lumbar puncture, also known as a spinal tap, you typically lie on your side with your knees drawn up to your chest. Then a needle is inserted into the spinal canal in your lower back to collect cerebrospinal fluid for testing.
Acute myeloid leukemia diagnosis often begins with an exam that checks for bruising, bleeding in the mouth or gums, infection, and swollen lymph nodes. Other tests include blood and lab tests, bone marrow biopsy, lumbar puncture, and imaging.
Tests and exams to diagnose acute myelogenous leukemia, also called AML, include:
Blood tests
Blood tests for acute myelogenous leukemia might include a test to count the number of blood cells in a sample of blood. This test is called a complete blood count. The results may show too many or too few white blood cells. Often the test finds that there are not enough red blood cells and not enough platelets. Another blood test looks for immature white blood cells called myeloblasts in the blood. These cells typically aren't found in the blood. But they can occur in the blood of people with AML.
Bone marrow aspiration and biopsy
Bone marrow aspiration and biopsy are procedures that involve collecting cells from the bone marrow. In bone marrow aspiration, a needle is used to draw a sample of the bone marrow fluid. In a bone marrow biopsy, a needle is used to collect a small amount of solid tissue. The samples are typically taken from the hip bone. The samples go to a lab for testing.
In the lab, tests can look for DNA changes in the bone marrow cells. Which DNA changes are present in your bone marrow cells are an important part of diagnosing AML. The results can help your healthcare team create a treatment plan.
Lumbar puncture
Sometimes, a lumbar puncture may be needed if there's concern that the leukemia has spread to the brain and spinal cord. A lumbar puncture also is called a spinal tap. It removes a sample of the fluid that surrounds the brain and spinal cord. A small needle is inserted into the lower back to remove a fluid sample. The sample is sent to a lab.
Imaging tests
Imaging tests make pictures of the body. For AML, imaging tests might make pictures of the brain, if there's concern that the leukemia cells have spread there. Imaging might include CT or MRI. If there's concern that the leukemia might have spread to another part of the body, imaging might be done with a positron emission tomography scan, also called a PET scan.
Your AML subtype
If you're diagnosed with AML, you may need further lab tests to determine your AML subtype. These tests include examining your blood and bone marrow for genetic changes and other signs that indicate specific AML subtypes. Currently, there are 15 different subtypes. Your AML subtype helps your healthcare professional determine the best treatment for you.
Treatment
Many types of treatment exist for acute myelogenous leukemia, also called AML. Treatment depends on several factors, including the subtype of the disease, your age, your overall health, your prognosis and your preferences.
Treatment usually has two phases:
- Remission induction therapy. This first phase aims to kill the leukemia cells in your blood and bone marrow. But it doesn't usually destroy all the leukemia cells. You will need further treatment to keep the disease from coming back.
- Consolidation therapy. This phase also is called post-remission therapy or maintenance therapy. It aims to kill the remaining leukemia cells. Consolidation therapy is crucial to helping lower the risk of relapse.
Treatments include:
Chemotherapy. Chemotherapy treats cancer with strong medicines. Most chemotherapy medicines are given through a vein. Some come in pill form. Chemotherapy is the main type of remission induction therapy. It also may be used for consolidation therapy.
People with AML usually stay in the hospital during chemotherapy treatments because the medicines kill many healthy blood cells while destroying leukemia cells. If the first chemotherapy cycle doesn't cause remission, it can be repeated.
Side effects of chemotherapy depend on the medicines you're given. Common side effects are nausea and hair loss. Serious, long-term complications may include heart disease, lung damage, fertility problems and other cancers.
Targeted therapy. Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die. Your leukemia cells will be tested to see if targeted therapy may be helpful for you. Targeted therapy may be used alone or in combination with chemotherapy during induction therapy.
Bone marrow transplant. A bone marrow transplant, also called a bone marrow stem cell transplant, involves putting healthy bone marrow stem cells into the body. These cells replace cells hurt by chemotherapy and other treatments. A bone marrow stem cell transplant may be used for both remission induction and consolidation therapy.
Before a bone marrow transplant, you receive very high doses of chemotherapy or radiation therapy to destroy your leukemia-producing bone marrow. Then you receive infusions of stem cells from a compatible donor. This is called an allogeneic transplant.
There is an increased risk of infection after a transplant.
Clinical trials. Some people with leukemia choose to enroll in clinical trials to try experimental treatments or new combinations of known therapies.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
No alternative treatments have been found to treat acute myelogenous leukemia. But integrative medicine may help you cope with the stress of a cancer diagnosis and side effects of your treatment.
Alternative treatments that may help relieve symptoms include:
- Acupuncture.
- Exercise.
- Massage.
- Meditation.
- Relaxation activities, such as yoga.
- Art and music therapy.
Coping and support
Acute myelogenous leukemia is a fast-growing cancer that requires quick decision-making. The following tips and resources may help you cope:
-
Learn enough about acute myelogenous leukemia to make decisions about your care. The term leukemia can be confusing because it refers to a group of cancers that aren't all that alike except that they all affect the bone marrow and blood.
You can waste a lot of time researching information that doesn't apply to your kind of leukemia. To avoid that, ask your doctor to write down as many details as possible about your specific disease. Then narrow your search to that disease.
Look for information at your local library and on the internet. You can start your information search with the National Cancer Institute and the Leukemia & Lymphoma Society.
- Lean on family, friends and others. Having a support system can help you cope. Get support from people close to you, a formal support group or others coping with cancer.
- Take care of yourself. It's easy to get caught up in tests, treatments and procedures. But it's important to take care of yourself, not just the cancer. Try to make time for cooking, watching sports or other favorite activities. Get plenty of sleep, see friends, write in a journal and spend time outside if you can.
- Stay active. Receiving a diagnosis of cancer doesn't mean you have to stop doing the things you enjoy. If you feel well enough to do something, do it. Check with your healthcare professional about starting any exercise program.
Preparing for your appointment
Make an appointment with your healthcare professional if you have symptoms that worry you. You may be referred to a doctor who specializes in blood cell diseases. This type of doctor is called a hematologist.
Appointments can be brief, and there's a lot of information to discuss. It's a good idea to be prepared. Here's some information to help you get ready:
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet before testing.
- Write down any symptoms you're experiencing, including those that may not seem related to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you're taking.
- Consider taking a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who comes with you may remember details that you missed or forgot.
- Write down your questions.
Your time with your healthcare professional is limited, so preparing a list of questions can help make the most of your time together. List your questions from most to least important in case time runs out. For acute myelogenous leukemia, some basic questions to ask include:
- What is likely causing my symptoms?
- What are other possible causes for my symptoms?
- Will I need more tests? Which ones?
- Will I need treatment?
- What are my treatment options?
- What are the potential side effects of each treatment?
- Is there one treatment you believe is best for me?
- I have these other health conditions. How will they affect my treatment and disease?
- How will treatment affect my daily life? Can I keep working?
- How long will treatment last?
- Are there any restrictions that I need to follow?
- Should I seek a second opinion?
- Is there a generic alternative to the medicine you're prescribing?
- Are there brochures or other printed material that I can take with me? What websites do you suggest?
In addition to the questions that you've prepared, don't hesitate to ask other questions.
What to expect from your doctor
Your healthcare professional is likely to ask you questions. Being ready to answer them may give you more time to go over other questions you have. Questions may include:
- When did your symptoms start?
- Do you have symptoms all the time or occasionally?
- How severe are your symptoms?
- What, if anything, improves your symptoms?
- What, if anything, worsens your symptoms?
What you can do in the meantime
Avoid activities that worsen your symptoms. For instance, try to take it easy if you're feeling very tired.
Dec. 20, 2024