概述
放射疗法使用高能射线或粒子杀死癌细胞。放射疗法也称为放疗,可作为前列腺癌的唯一治疗方法。此外,也可以与其他治疗方法联合使用,例如化疗或手术。
可在体内或体外对前列腺癌进行放疗。
外照射疗法(EBRT)是一种用于治疗前列腺癌的常见放射疗法类型。在 EBRT 期间,一台大机器绕身体外部移动,将辐射束定向照射至身体的特定部位。
外照射疗法最常使用 X 线,但也可能使用其他类型的放射疗法,包括质子束放射疗法。
近距离放射治疗是一种体内放射治疗。因此有时又称为内照射治疗(IRT)。在近距离放射治疗中,会将一个小型放射性装置放置在前列腺内或附近,将放射线直接照射至治疗部位。
您可能会接受一种或两种放射疗法。医疗护理团队会向您解释这些疗法及其潜在风险和益处。你们可以共同决定放射疗法是否是最适合您的治疗方法。
目的
医疗护理团队可能通过以下几种方式实施前列腺癌放疗:
- 作为早期前列腺癌(有时是晚期前列腺癌)的唯一治疗方法。 对某些患者来说,放疗可能是唯一的治疗方法。
- 术后采用该疗法以降低癌症复发的风险。 辐射可能有助于消除可能残留的任何癌细胞,并降低癌症扩散或复发的风险。以这种方式使用的放疗又称为辅助治疗。
- 如果癌灶未完全清除或者癌症复发于前列腺,则在术后采用该疗法。 这也称为前列腺癌挽救性放疗(SRT)。
- 作为更严重或更晚期癌症整体治疗计划的一部分。 这些可能包括已生长至前列腺外并扩散至身体其他部位的癌症。针对这类癌症,除手术或其他治疗外,可能采用放疗以延缓癌症生长。还可能有助于预防或缓解癌症扩散到前列腺外所引发的症状,如骨痛。
常见疑问包括:哪种癌症治疗方法最适合您?应单独采用放疗,还是联合进行其他治疗? 您可能还想知道外照射疗法或近距离放射治疗是否是放疗的正确选择。
最佳治疗方案取决于您所患前列腺癌的类型、确切位置和分期。医护团队将针对您的具体情况,与您共同制定合适的治疗方案。
风险
放射疗法是治疗前列腺癌的方法,多数情况下是安全有效的。一些现代放疗技术能够将能量射束精准定向攻击癌细胞,有助于保护健康组织免受高剂量辐射的影响。
但放疗在破坏癌细胞的同时,也可能损伤健康细胞,并且还可能带来一些副作用。这些副作用取决于多项因素,包括您接受的放疗类型、剂量以及暴露于辐射的健康组织范围。
前列腺癌放疗的多数副作用轻微且是一过性的,并且在治疗结束后会随时间推移逐渐改善。
前列腺癌放射疗法的副作用可能包括:
泌尿系统副作用。 放射疗法可能刺激膀胱基部或阴茎等周围器官。可能导致尿频、排尿困难或血尿等症状。这些症状通常在开始放疗后 2 至 3 周内开始出现,并在放疗结束后 3 个月内消退。
肠道副作用。 前列腺癌放疗可能刺激肠道,从而可能导致腹泻、便频、便急、血便或排便不尽感。
性功能相关副作用。 部分前列腺癌患者在放疗后出现勃起困难或难以维持勃起。这种状况被称为勃起功能障碍。但未接受放疗的前列腺癌患者的长期勃起功能恢复率与之相近。
疲劳。 放疗期间,您可能会感到极度疲倦。这种情况可能持续至治疗后数周或数月。
皮肤反应。 如果接受外照射疗法,身体治疗部位的周围皮肤可能出现类似晒伤的红肿和疼痛。
继发性癌症。 接受放疗的前列腺癌患者患某些其他癌症(包括膀胱癌或胃肠道癌)的风险略有增加。
这些副作用可能不同于质子束放疗的副作用
由于放射疗法专业人员能够更好地控制质子束疗法释放最高能量浓度的位置,因此该疗法对健康组织的影响较小,副作用也比其他形式的放射疗法更少。然而质子疗法仍会向健康组织释放部分辐射,因此可能会产生副作用。
近距离放射治疗的特定风险和副作用
虽然近距离放射治疗的许多风险和副作用与 EBRT 相似,但仍存在一些关键差异。
如果是接受临时近距离放射治疗,阴囊与直肠之间的部位可能在治疗后感到疼痛、压痛或肿胀,持续大约一周时间。还可能观察到尿液呈深红褐色。此外,可能略有更高风险出现尿潴留,即可能无法完全排空膀胱或出现排尿困难。
如果进行永久性近距离放射治疗,放射性植⼊物会持续数周或数月释放微量辐射。医护团队可能会建议您在这一期间远离孕妇和幼儿,以防万一。如果您乘坐飞机,机场安检系统可能检测到这种辐射。您可以向医疗护理专业人员索要治疗说明文件。
某些近距离放射治疗植入物可能会脱离植入位置,但这种风险很小。进行性活动时使用避孕套,可以防止将植入物传递给伴侣。
医疗护理团队可能会要求您将尿液过滤一小段时间。如果要这样做,医疗护理团队会指导安全操作方法。
放射治疗期间激素治疗的副作用
在前列腺癌放疗前或期间,医疗护理团队可能建议采用激素治疗以降低睾酮或双氢睾酮水平。这是因为这些激素(称为雄激素)会促进前列腺癌细胞生长。
降低雄激素水平或阻止其进入前列腺癌细胞,可能让肿瘤缩小或延缓生长。
您可能在放疗之前接受激素治疗以缩小癌灶;或者,如果癌症复发风险较高,您也可能在放疗的同时接受激素治疗。如果癌灶未完全切除或者癌症复发,您可能在放疗后接受激素治疗。
对比单独放疗,放疗期间联合进行激素治疗可能会带来更多副作用。激素治疗的常见副作用包括:
- 性功能副作用,如勃起功能障碍或性欲低下。
- 潮热。
- 疲劳。
- 性欲减退。
较少见的副作用可能包括体重增长、肌质量减少、胆固醇水平升高、抑郁、红细胞计数降低(又称为贫血),以及睾丸和阴茎萎缩。
一旦停止激素治疗,这些症状通常会随着时间的推移而改善。请询问医疗护理团队您在治疗期间和治疗后最有可能出现的副作用。
如果发生了激素治疗的副作用,医疗护理团队可能建议您采用预防或治疗这些副作用的治疗方法。这些治疗方法可能包括药物治疗。
如何进行准备
前列腺癌放射疗法的计划制定过程取决于您接受的治疗类型。
外照射疗法的准备
在前列腺癌外照射疗法开始前,医疗护理团队将指导您完成计划环节。这有时称为放疗模拟定位。
该计划环节有助于医护团队精确制定放疗计划,确保安全准确地向体内所需部位递送辐射。
治疗计划通常包括:
完成计划过程后,放疗团队会根据您的癌症分期、整体健康状况和治疗目标来确定 EBRT 类型和照射剂量。
质子束疗法的特别注意事项
由于质子束疗法成本较高,有些保险计划不承保该项治疗。如果您的医护团队建议采用质子束疗法,请咨询您的医疗保险提供方,了解哪些费用属于承保范围以及哪些费用需要自付。
近距离放射治疗的准备
在前列腺癌内照射放疗开始前,您需要与医护团队成员会面以制定治疗计划。您可能还需要进行影像学扫描,例如计算机体层成像(CT)或磁共振成像(MRI),以确定待治疗的前列腺确切部位。
制定治疗日程计划
您通常能够自行开车往返放疗就诊处。但如果您在治疗期间感到疲劳或不适,最好在后续治疗中安排他人接送。
请穿着易脱的衣物,因为您可能需要换上病号服。
请勿在骨盆部位使用爽身粉、体香剂或胶布绷带。
如果您正在接受持续数周的放疗,则您可能需要为治疗请假。请与医疗护理团队沟通预期情况以便制定计划。
可能出现的情况
术中
前列腺癌放射疗法的流程因您接受的辐射治疗类型而异。
外照射疗法
外部束辐射治疗前列腺癌
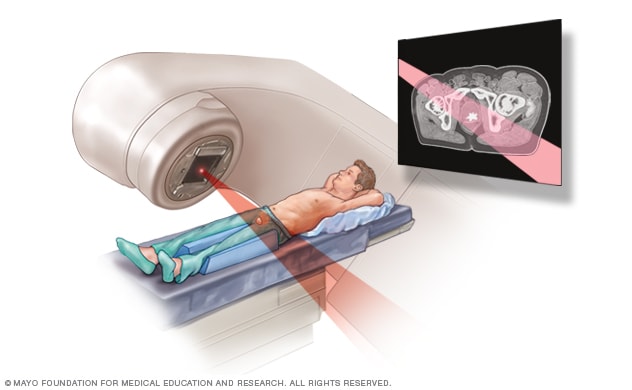
外部束辐射治疗前列腺癌
During external beam radiation treatment for prostate cancer, you lie on a table while a linear accelerator moves around you to deliver radiation from many angles. The linear accelerator delivers the precise dose of radiation planned by your treatment team.
前列腺癌外照射疗法(EBRT)使用直线加速器或质子设备向身体定向发射辐射束。每次治疗期间,该设备会根据治疗团队制定的方案精确递送辐射剂量。能量束可能由 X 线、质子或其他类型的能量构成。
EBRT 通常在门诊进行,每周五天,持续数周。部分医疗中心提供短疗程放射疗法治疗方案。例如,您可能在较短的天数内获得较高剂量的辐射。该方案称为低分割放射治疗。
医疗护理团队可能建议采用特定类型的外照射疗法,例如:
- 调强放射治疗(IMRT)。 这是最常见的前列腺癌外照射疗法类型。IMRT 可实现辐射束的精确塑形以匹配癌灶形态。辐射束的强度可以调整。这样可以精确控制放射治疗。
- 立体定向体部放射治疗(SBRT)。 这种 EBRT 采用先进 3D 或 4D 成像和高聚焦辐射束,可实现精准高剂量照射。由于单次剂量高于传统放疗,因此一个完整的治疗周期通常可以在 1 至 5 次疗程内完成。根据治疗设备的名称,SBRT 也可能被称为伽玛刀或 X 刀放疗。
- 立体定向体部质子疗法(SBPT)。SBPT 将 SBRT 技术与质子疗法相结合。SBPT 期间可能使用一种被称为组织间隔物的凝胶状物质。该凝胶帮助在前列腺与直肠之间创造更多间隙,从而更安全地靶向前列腺放疗,减少对直肠健康组织的辐射。组织间隔物会逐渐自然溶解。
- 质子束治疗。 质子束治疗是一种新型放疗技术,利用高能量束治疗癌症。该治疗方法不使用 X 线束,而是采用带正电粒子(称为质子)所产生的能量。由于质子束极其精准,可在减少健康组织损伤的同时递送更高辐射剂量。
每次治疗时间通常不到一小时。其中大部分时间用来做准备。放射治疗本身仅需几分钟。
在治疗过程中:
- 您将躺在治疗台上,并采用您在放射治疗计划期间练习的体位。
- 可能放置特殊的垫枕或垫块,以帮助您在每次放射治疗期间保持相同的体位。
- 直线加速器可能会围绕您的身体旋转,从不同的方向递送辐射束。在此过程中,您需要静卧并正常呼吸。
- 放射疗法团队会待在隔壁的房间,通过视频和音频设备观察您并与您进行交流。
整个治疗过程应该不会引发疼痛。尽管您能看到直线加速器移动,但无法感知或看到辐射进入体内。如果您在治疗过程中的任何时候感到不适,请及时告知放疗团队。他们可协助调整至更舒适的体位。
近距离放射治疗
永久性前列腺近距离治疗
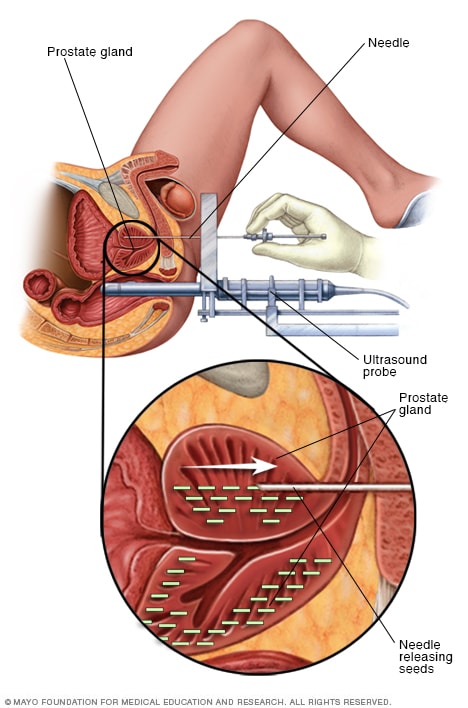
永久性前列腺近距离治疗
永久性前列腺近距离治疗包括在前列腺内放置许多放射性粒子来治疗前列腺癌。手术期间,将在直肠中放置一个超声探头,以帮助引导放置粒子。粒子将发出辐射,这种辐射会在几个月后消失。
近距离放射治疗通过将放射源置于体内癌灶附近,可精准递送所需辐射剂量。由于近距离放射治疗可以一次性安全地递送更高的辐射剂量,因此可缩短总体治疗时间。
在近距离放射治疗中,会将米粒大小的固态放射性装置植入前列腺。超声或其他影像学检查技术可用于引导放射学装置准确定位。这些图像有助于确保治疗在正确的位置进行。随后,放射性装置将递送所需的精准辐射剂量。
近距离放射治疗可分为短期治疗的临时性近距离放射治疗,或永久植入体内的永久性近距离放射治疗。
临时性近距离放射治疗。 这有时也称为高剂量率(HDR)近距离放射治疗。
进行临时性近距离放射治疗时,会将高剂量放射性物质短时间置入前列腺,时间通常为 5 至 20 分钟。
您可能会在数天内接受一至两次临时性近距离放射治疗。每次治疗后放射性物质将被取出。
临时性近距离放射治疗期间:
- 您以舒适姿势平卧于治疗台上。
- 根据治疗方案,您可能需要接受麻醉以便于医疗程序的实施。
- 放疗团队会将辐射递送装置(通常为简易导管或细针)放置在阴囊和肛门之间,并放入前列腺。
- 随后通过机器辅助将小型放射源植入前列腺。
- 放疗团队会到隔壁的房间,通过视频和音频设备观察您,并与您进行交流。如果您在近距离放射治疗期间感到不适或有任何顾虑,可以告知医护团队。
一旦团队将放射性物质从您的身体里移除,您就不会释放放射物或具有放射性。您可以继续进行日常活动。
永久性近距离放射治疗。 这有时也称为低剂量率(LDR)近距离放射治疗。在永久性近距离放射治疗期间,放射性物质会留在体内。这是前列腺癌的常见治疗方法。
永久性近距离放射治疗期间:
- 您接受了麻醉,因此在手术过程中您不会感到不适。
- 放疗团队将小型放射性装置通过肛门和阴囊之间的部位放入前列腺中。
- 影像学检查(如超声或 CT)可能用于确保将放射性物质放置在正确的位置。
只要这些小型放射性装置放置正确,就不会有任何不适。
您身体的治疗部位会释放出低剂量的辐射。这种辐射会逐渐减弱,直至消失。虽对他人风险较低,但您可能需要在术后数日内避免与儿童和怀孕者密切接触。
术后
放疗结束后,需定期复诊,由医护团队为您评估治疗效果。医护团队可能会建议您接受扫描或血液检测来帮助评估治疗效果。
治疗后您可能恢复大多数日常活动,包括工作和开车。但需注意以下几点:
- 工作。 许多患者在接受前列腺癌放疗期间会继续工作。如果治疗导致您感到疲劳,在可能的情况下可考虑请几天假、调整日程或工作量。如果您出现泌尿道或肠道副作用,可与雇主协商增加休息频次。
- 驾驶。 如果您在治疗后感到极度疲倦,或者您正在服用使您嗜睡的药物,为安全起见,治疗结束后请让可信赖者开车送您回家。
- 性别。 对大多数人而言,治疗期间及治疗后进行性活动是安全的。如果您正在接受永久性近距离放射治疗,医疗护理团队可能建议您使用避孕套。
- 运动。 研究表明,放疗后进行适度运动是安全的,甚至可能有助于减轻癌症相关的疲劳。
如果接受永久性近距离放射治疗
植入前列腺内或附近的装置会在短时间内持续释放辐射。辐射通常局限于治疗区域附近,因此不太可能影响他人。作为预防措施,医疗护理团队可能建议您在几天内限制访客,尤其是儿童和怀孕者。
结果
放射疗法结束后,您需要定期前往医疗护理团队处复诊。您可能需要接受影像学检查或血液检测以评估放疗效果。
血液检测可以测定血液中的前列腺特异性抗原(PSA)水平。这些检查可帮助医疗护理专业人员评估治疗是否成功。
您可咨询医疗护理专业人员何时能获知疗效评估结果。
前列腺癌放疗成功率
前列腺癌放疗的成功率取决于多个因素,包括癌症分期和侵袭性、患者健康状况和年龄以及整体治疗方案。
前列腺癌放疗非常有效,与针对较高风险癌症的激素治疗联用时尤其有效。大多数患者的癌灶会缩小或消失。
治愈率非常高,特别是低风险和中风险前列腺癌患者。高风险前列腺癌患者的治愈率也较为乐观,但与癌症扩散程度直接相关。
在一项大型研究中,接受放疗的前列腺癌患者 10 年生存率从 90% (高风险癌症)到 98% (低风险癌症)不等。
Dec. 13, 2025