诊断
淋巴瘤的常见问题解答
血液学家医学博士 Stephen Ansell 解答有关淋巴瘤最常见的问题。
很多时候我们其实并不清楚这种疾病的诱因。但我们清楚地知道患者细胞内发生了一些变化。我们能看到细胞在基因层面发生了变化。随着这种变化的发生,这些细胞以超出其应有的生长速度快速生长,并且它们可能一直存活,而不会自然凋亡。这会导致它们随着时间的推移而慢慢积聚。但究竟是什么导致了这种基因变化,我们还不得而知。
虽然家族成员更可能罹患这种疾病,但它不是一种家族遗传性疾病。我们认为某些易感基因可能会增加您患淋巴瘤的风险。但这种情况的发生需要满足一定的条件,通常来说是通过接触毒素、病毒或其他东西而触发的。
我认为明确治疗目标非常重要。低级别淋巴瘤的一个特点是很长时间后才会出现症状,并且需要相当长的时间才会危及患者的健康。但是,我们目前还没有找到这种癌症的治愈方法。相比于这种癌症本身的风险和副作用,我们还需要权衡治疗带来的潜在风险和副作用。因此,如果您罹患的癌症级别较低、生长缓慢,并且未表现出任何症状,我们可能会推迟治疗,只有在您确实需要的时候才进行治疗。
需要指出的是,化疗可能包含两个部分。一部分是靶向癌症的化疗,也就是化学药物治疗;另一部分是针对癌症或淋巴瘤细胞外的蛋白质的免疫疗法,也就是抗体治疗。化疗的目的是杀死快速生长的癌细胞,这对于治疗淋巴瘤来说是一件好事,因为这些癌细胞的生长速度通常极快。然而这也会带来一个挑战,因为很多健康细胞也可能会快速生长。正如我刚才提到的,免疫疗法通过结合或攻击细胞外的蛋白质来发挥作用。但某些淋巴瘤细胞的蛋白质与某些正常细胞相同。如此一来,正常细胞也可能被误杀。另外,由于该疗法的一种潜在副作用,您的免疫系统也可能受到些许抑制。
虽然我也希望这是真的,但遗憾的是,这种说法并不完全正确。目前还没有能够直接靶向或针对淋巴瘤细胞的膳食或运动治疗方案。但总的来说,健康均衡的饮食和良好的运动习惯能够改善您的整体健康状况,提高您的免疫系统功能,让您能够耐受化疗,并帮助您更好地对抗癌症。好消息是,大量研究表明,身体健康的患者接受淋巴瘤治疗的效果通常更好。听到这个消息,您是不是有了更多的动力去采用健康饮食和定期锻炼了呢?
请尽可能多地了解相关信息。与您的医生、护士、PA 以及治疗团队中的其他人员合作,多向他们进行咨询。我们的最终目标是尽可能为您提供最好的治疗结果。因此,您与治疗团队共享信息对于您的治疗以及我们所期待的最佳结果都至关重要。
骨髓检查
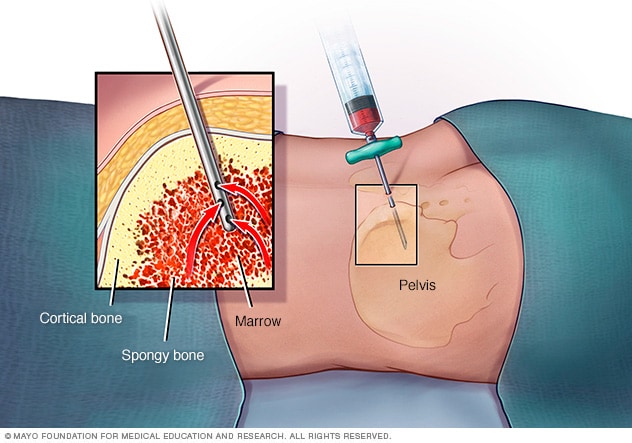
骨髓检查
骨髓穿刺时,医疗护理专业人员使用一根细针抽出少量液体骨髓。通常从髋骨(骨盆)后方的某个部位抽取。通常会同时进行骨髓活检。这项医疗程序需要取出一小块骨组织和其中包含的骨髓。
诊断淋巴瘤时,常常首先检查颈部、腋下和腹股沟有无淋巴结肿大。其他检查包括影像学检查和采集一些细胞进行检测。用于诊断的检查类型可能取决于淋巴瘤的位置和您的症状。
体格检查
医务人员可能会先询问您的症状。另外也可能会询问您的健康史。
接下来,医务人员可能会触摸并按压您身体的某些部位,以检查是否有肿胀或疼痛。为了找到肿大的淋巴结,医务人员可能会触摸您的颈部、腋下和腹股沟。如果您感到有肿块或疼痛,一定要说出来。
Imaging tests
Imaging tests make pictures of the body. They can show the location and extent of lymphoma. Tests might include MRI, CT and positron emission tomography (PET) scans.
活检
活检医疗程序采集组织样本并在实验室中进行检测。对于淋巴瘤,活检通常包括切除一个或多个淋巴结。淋巴结随后会被送至实验室进行检测,以查看是否存在癌细胞。其他特殊检查可提供更多有关癌细胞的信息。医护团队会使用此信息为您制定治疗计划。
影像学检查
医疗护理团队可能建议您接受影像学检查,以寻找体内其他部位是否有淋巴瘤体征。检查可能包括 CT、MRI 和正电子发射体层成像扫描(即 PET 扫描)。
Lumbar puncture
A lumbar puncture is a procedure to collect fluid from around the spinal cord. A lumbar puncture, also called a spinal tap, uses a needle. A healthcare professional inserts the needle between two bones in the lower back and draws out some of the fluid that surrounds the brain and spinal cord. This fluid is called cerebrospinal fluid. The fluid goes to a lab where it's tested for cancer cells.
For lymphoma, a lumbar puncture may be done if you have neurological symptoms. It also may be done if you are at higher risk of lymphoma of the central nervous system.
Upper endoscopy
An upper endoscopy is a procedure to look at the inside of the esophagus, stomach and first part of the small intestine. A thin, tubelike instrument with a light and a lens for viewing, called an endoscope, is inserted through the mouth and passed down the throat. Tools are passed through the tube to remove a sample of tissue for testing. It may be used if your healthcare professional thinks you have lymphoma in the stomach.
Testing lymphoma cells in the lab
Lymphoma cells collected from a biopsy or a bone marrow aspiration and biopsy go to a lab for testing. In the lab, specialized tests look for specific things about the cells. The healthcare team uses the results to find out the type of lymphoma that you have.
To learn whether the cells are Hodgkin lymphoma cells, the healthcare professionals in the lab look for:
- Proteins on the surface of the cancer cells. Lymphoma cells have certain proteins on their surfaces that help identify them. These proteins are known as markers. These markers can help identify the type of lymphoma.
- Changes in the cancer cell DNA. Cancer happens when cells get changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. Some lymphomas have a gene change that causes their DNA to rearrange. This is known as translocation. Some genes also may be missing parts of their DNA, called deletion. These gene changes cause the cells to multiply rapidly.
治疗
淋巴瘤有多种治疗方法。这包括放疗、化疗、免疫疗法、靶向治疗和骨髓移植(也称为干细胞移植)。有时会使用不同治疗的组合。最适合您的治疗方法取决于您所患的淋巴瘤类型。
可能不需要立即开始治疗
淋巴瘤不一定需要立即开始治疗。有些类型的淋巴瘤生长非常缓慢。您和医务人员可以决定等到癌症开始产生症状后再进行治疗。
如果不接受治疗,您需要定期与医务人员约诊,以监测症状。
化疗
化疗使用强效药物来治疗癌症。多数化疗药物通过静脉给药。有些则是药片形式。治疗淋巴瘤时,通常会使用两种或多种药物联合治疗。
免疫疗法
癌症免疫疗法是一种药物疗法,可以帮助人体的免疫系统杀死癌细胞。免疫系统通过攻击病菌和其他不应该出现在人体内的细胞来对抗疾病。癌细胞通过躲避免疫系统的攻击而存活。免疫疗法帮助免疫系统细胞找到并杀死癌细胞。免疫疗法可以用于多种类型的淋巴瘤。
放射疗法
放射疗法用强大的能量束来治疗癌症。能量来自 X 线、质子或其他来源。在放射疗法中,您需要躺在治疗台上,同时有一台大型机器在您身体周围移动。机器向您身体内的精确点位发送放射线。
靶向治疗
癌症靶向治疗是一种利用药物攻击癌细胞中特定化学物质的治疗方法。通过阻断这些化学物质,靶向治疗可杀死癌细胞。医生可能对您的淋巴瘤细胞进行检测,以了解靶向治疗是否可能对您有帮助。
Clinical trials
Clinical trials are studies of new treatments. These studies provide a chance to try the latest treatments. The risk of side effects might not be known. Talk with your healthcare team about the possibility of joining a clinical trial.
CAR T 细胞疗法
嵌合抗原受体(CAR)T 细胞疗法又称 CAR T 细胞疗法,训练人体的免疫系统细胞对抗淋巴瘤。这种疗法首先从血液中取出一些白细胞,包括 T 细胞。然后将这些细胞送往实验室。在实验室中对这些细胞进行处理,让其识别淋巴瘤细胞。细胞随后被注回您的体内。然后可以找到并破坏淋巴瘤细胞。
Bone marrow transplant
A bone marrow transplant, also called a bone marrow stem cell transplant, involves putting healthy bone marrow stem cells into the body. These cells replace cells hurt by chemotherapy and other treatments. Stem cells can come from your own body, called an autologous transplant. Stem cells also can come from a donor, called an allogeneic transplant.
A bone marrow transplant may only be an option for some types of lymphoma and for people who are younger and in good health. Chemotherapy is typically done before the transplant to suppress the immune system and bone marrow.
Treatments for cutaneous lymphomas
Treatments for cutaneous lymphomas may include topical medicines and phototherapy. Topical medicines are placed directly on the patches or plaques on the skin. They may include corticosteroids, retinoids and topical chemotherapy. Phototherapy uses lights combined with medicines to treat some cancers of the skin.
Monitoring after treatment
After treatment is complete, you may have frequent follow-up appointments to see if the cancer has come back, known as a relapse. You may have repeat blood and imaging tests and, if needed, biopsies, to check for relapse.
Side effects of treatment
Treatments for lymphoma may have side effects. These may include nausea, vomiting, fatigue, fever, rash, diarrhea, infection and more.
Harmful side effects from treatments may include:
- Bone marrow suppression. When the bone marrow is suppressed, it can't produce enough blood cells, including white blood cells. White blood cells help fight infections, so with a lower amount, you are at a higher risk of infections.
- Febrile neutropenia. Febrile neutropenia is a serious condition that can happen in people being treated for cancer. Febrile means having a fever. Neutropenia means having a low number of neutrophils, which are a type of white blood cell that helps fight infections. In febrile neutropenia, the body is trying to fight an infection but doesn't have enough neutrophils.
- Medicine toxicity. Some medicines used to treat cancer can be harmful to the body. They can cause organ damage and other issues. Whether a medicine is toxic depends on the type and how much you take. There are many different medicine options. Your healthcare team can work with you to find the best medicines for you.
- Reactivating viruses. If you have had a viral infection in the past such as hepatitis B or hepatitis C, some treatments can cause the virus to become active again. This can lead to liver inflammation, liver damage and other complications.
- Tumor lysis syndrome. Tumor lysis syndrome is a serious condition that can happen when cancer cells break down quickly after treatment. When these cells die, they release substances into the bloodstream that can overwhelm the body. This can lead to issues with the kidneys and other organs. You may take medicines to treat or prevent harmful side effects.
- Infertility. Some lymphoma medicines can cause issues with fertility. If you are concerned about fertility, talk about your options with your healthcare professional before beginning treatment.
临床试验
探索 Mayo Clinic 的研究 测试新的治疗、干预与检查方法,旨在预防、检测、治疗或控制这种疾病。
妥善处理与支持
确诊淋巴瘤可能让人难以接受。随着时间的推移,您会找到办法应对确诊淋巴瘤常常带来的压力和不确定性。在那之前,您可能会发现以下事情有帮助:
了解淋巴瘤。
如果您想了解更多有关您淋巴瘤的信息,请向医护团队咨询您癌症的详情。询问癌症类型和您的预后。索取了解有关您治疗方案最新信息的可靠来源。详细了解癌症状况和治疗方案后,您在做出治疗决策时会更加自信。
与朋友和家人保持亲密关系
朋友和家人能够带来情感支持,也能提供您需要的实际支持,例如在您住院期间帮助您打理家务。
找人倾诉
找到一个愿意听您诉说希望和恐惧的倾听者。这可以是您的朋友或家人。咨询师、医务社工、神职人员或者癌症互助团体的关心和理解,可能也会对您有所帮助。向医务人员咨询您所在地区的互助小组。您还可以联系癌症组织,例如美国国家癌症研究所或白血病和淋巴瘤协会。
在推特上关注我们
@MayoCancerCare
准备您的预约
如果出现任何令人担忧的症状,请与医生或其他医务人员约诊。如果医务人员怀疑您患有淋巴瘤,可能将您转诊给擅长治疗血细胞疾病的医生。这类医生称为血液科医生。
就诊时间可能很短,而且有很多事情需要谈论。最好提前做好准备。以下信息有助于做好准备,并了解将会发生什么:
您可以做什么
- 了解就诊前是否有任何限制规定。约诊时,询问是否需要提前做准备,比如限制饮食。
- 写下您目前的所有症状,包括看似与您本次约诊原因无关的任何症状。
- 写下关键个人信息,包括任何重大压力或近期的生活变化。
- 列出您正在服用的所有药物、维生素或补充剂。
- 考虑让家人或朋友陪同就诊。有时,您可能难以记住就诊时医务人员告知的所有信息。陪同者可能会记住您遗漏或忘记的一些事项。
- 写下需要向医疗护理专业人员咨询的问题。
由于向医务人员咨询的时间有限,因此提前列出问题有助于充分利用就诊时间。请按照重要程度由高而低的顺序列出问题,以免时间不够。对于淋巴瘤,要咨询的一些基本问题包括:
- 我患上淋巴瘤了吗?
- 是哪种类型的淋巴瘤?
- 我的淋巴瘤处于哪个阶段?
- 我的淋巴瘤是侵袭性还是缓慢进展?
- 我是否需要做更多检查?
- 我需要接受治疗吗?
- 有哪些可选的治疗方案?
- 每种治疗方法都有哪些潜在的副作用?
- 治疗对我的日常生活有什么影响?我可以继续工作吗?
- 治疗需要多长时间?
- 有没有您觉得最适合我的治疗方案?
- 如果您的亲友出现我这种情况,您会给出什么建议?
- 我需要去看淋巴瘤专科医生吗?费用是多少?我的保险能报销吗?
- 有没有可以拿回去参考的手册或其他印刷材料?您是否可以推荐一些网站?
就诊期间,您可以随时提出其他任何问题。
医生可能做些什么
医务人员可能会问您几个问题。请做好回答这些问题的准备,以便有更多的时间讨论您想解决的其他问题。医务人员可能会询问:
- 您第一次出现症状是什么时候?
- 症状是持续存在还是偶尔出现?
- 您的症状有多严重?
- 有没有什么因素有助于改善您的症状?
- 有没有什么因素会加重您的症状?
- 您家族中是否有人患过癌症,包括淋巴瘤?
- 您或您家族中是否有人患过免疫系统状况?
- 您或家人是否接触过毒素?
Dec. 20, 2024