Nov. 05, 2019
Many men ages 55 to 69 in the United States are advised to be screened annually or every other year for prostate cancer. Screening may consist of a blood test, prostate-specific antigen (PSA) and digital rectal exam (DRE). If the patient has a confirmed elevated or rising PSA, or an abnormal DRE, the next step is often to proceed with a transrectal ultrasound-guided prostate biopsy.
Transrectal approach to prostate biopsy
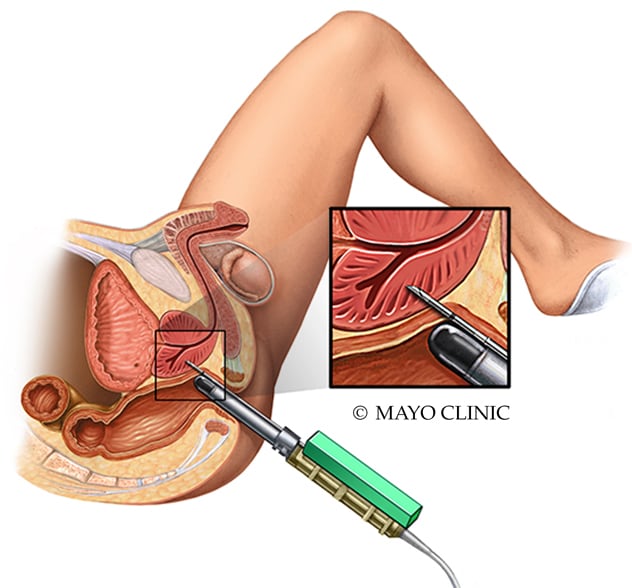
Transrectal approach to prostate biopsy
In the transrectal approach, the biopsy needle is passed through a needle guide attached to ultrasound, and then through the rectal wall into the prostate under guidance.
The overwhelming majority (99%) of prostate biopsies are conducted transrectally. Although this approach has been employed for many years, there are multiple downstream risks. Infections continue to be the greatest risk associated with prostate biopsies; the risk of sepsis, a severe life-threatening infection, is approximately 1 to 2 in 100. In addition, some areas of the prostate, including the anterior prostate, are undersampled with a systematic transrectal approach, which means that some clinically significant prostate cancers may be missed. Both of these problems can be addressed by performing the prostate biopsy via a transperineal approach.
Transperineal and transrectal biopsy needle course
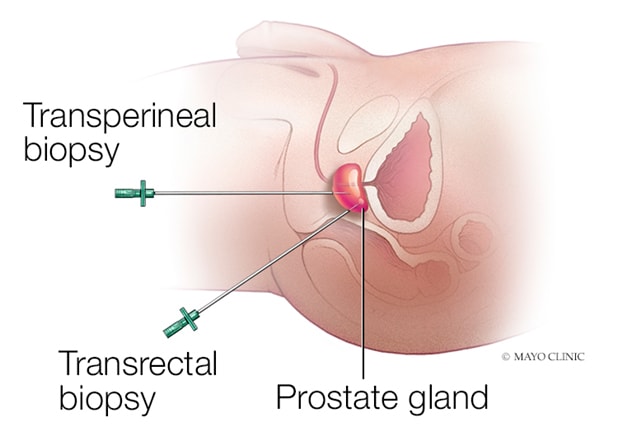
Transperineal and transrectal biopsy needle course
The needle passes through the perineal skin in the transperineal approach. In the transrectal approach, the biopsy needle passes through the rectal wall.
At Mayo Clinic's campus in Rochester, Minnesota, urologist Derek J. Lomas, M.D., Pharm.D., has chosen to discontinue routine use of the transrectal approach to prostate biopsy and now performs transperineal prostate biopsy. Dr. Lomas gained extensive experience with the technique during his fellowship training in London. "Mayo Clinic is one of a few centers in the region that perform high volumes of transperineal biopsy. This approach helps to accurately diagnose threatening infectious complications associated with prostate biopsy. It provides good diagnostic yield and is particularly well-suited for patients with previous infectious complications," says Dr. Lomas."
Overview of ultrasound-guided transperineal prostate biopsies
In transperineal biopsy, the urologist passes the biopsy needle through the perineal skin and into the prostate, rather than passing the biopsy needle through a potentially contaminated rectum. The biopsy needle is still guided by an ultrasound placed in the rectum. This approach lowers the risk of sepsis to 1 in 500, rather than the approximate 1 to 2 in 100 risk of sepsis related to transrectal biopsy.
"There are several different techniques by which we can perform transperineal biopsy," says Dr. Lomas. "The choice of technique is based on whether a fusion or a systematic biopsy is needed and if the patient is in the clinic or under sedation.
"The first technique uses a device called a stepper, which is used to cradle the ultrasound probe and provide a guidance grid for biopsy needle insertion. Urologists who have performed brachytherapy for prostate cancer would be familiar with this device. The downside of this approach is that each biopsy of the prostate requires a skin puncture, which limits the utility of this approach in the clinic where we are using local anesthesia only. This technique may still be used, but an excellent skin block is paramount."
Mayo Clinic urologists also employ the freehand approach, using the needle access guide. "In this approach, only one or two skin punctures are needed for each side of the prostate," says Dr. Lomas. "Through a needle access guide placed through the anesthetized skin of the perineum, the biopsy needle can be reintroduced for multiple biopsies without repeat puncture of the skin. The biopsy needles are guided by an ultrasound probe in the rectum. This approach allows for improved patient comfort in the clinic setting."
Transperineal biopsy is appropriate for all patients, but may specifically benefit patients with the following conditions:
- History of infection after a previous transrectal biopsy
- History of prostatitis
- Inflammatory bowel disease
- Rectal bleeding complications after previous biopsy
- Previous negative transrectal biopsy with suspicion of anterior prostate tumor
"Research so far suggests that the transperineal approach is noninferior in terms of diagnostic yield when compared to transrectal biopsy, although some studies do show a slightly higher detection rate with the transperineal approach," says Dr. Lomas. "The main benefit is safety, due to the lower risk of severe life-threatening infection. Also, with a transperineal approach it is much easier to access the anterior prostate, which is not well sampled with transrectal biopsy."
Complications associated with transperineal biopsy
There are several barriers to widespread adoption of the transperineal procedure. "Historically, transperineal biopsy has required sedation or general anesthesia. With increasing experience and novel techniques and equipment, we are now able to perform transperineal biopsy in our clinic setting using only a local anesthetic, although patients with large glands may still require sedation," says Dr. Lomas.
Risks associated with transperineal biopsy include:
- Infection such as sepsis (1 in 500 men)
- Blood in the urine (most men, mild )
- Blood in the semen (most men, lasting up to three months)
- Temporary erectile dysfunction (less than 5% of men)
- Bruising of the skin (most men, mild)
- Urinary retention requiring catheter placement (1% of men)
Notably absent from transperineal biopsy risk, when compared with transrectal biopsy risk, is rectal bleeding, since the needles are not going through the rectal wall.
"We are going to see a lot of changes in the pathway for diagnosing prostate cancer in the next decade," says Dr. Lomas. "The first change that we'll see here in the U.S. is likely the use of prostate MRI to help decide if a patient should have a prostate biopsy. With high-quality MRI, such as the MRI technology in use at Mayo Clinic, we may be able to safely avoid prostate biopsy in many men."
Data from the PROMIS trial, published in The Lancet in 2017, indicate that using multiparametric-MRI to triage men might allow 27% of patients to avoid a primary biopsy and reduce the number of clinically insignificant cancers diagnosed by 5%.
"European guidelines have changed to recommend MRI prior to prostate biopsy, but one barrier to using this MRI-first approach in the U.S. is that access to and insurance coverage for pre-biopsy prostate MRI is variable throughout the country," says Dr. Lomas. "The future is bright here in the U.S., however, as the American Urological Association (AUA) issued a new policy statement, published in the Journal of Urology in 2019, supporting the use of quality prostate MRI prior to a patient's first biopsy. With the support of the AUA, I think we will see significant increases in patient access this valuable test."
For more information
Ahmed HU, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): A paired validating confirmatory study. The Lancet. 2017;389:815.
Mottet N, et al. Prostate cancer guidelines. European Association of Urology.
Bjurlin MA, et al. Update of the AUA policy statement on the use of multiparametric magnetic resonance imaging in the diagnosis, staging and management of prostate cancer. Journal of Urology. In press.